

Copyright 2015 © Nigerian Journal of Paediatrics. All Rights Reserved. . Powered by Pelrox Technologies Ltd
ISSN 03 02 4660 AN OFFICIAL JOURNAL OF THE PAEDIATRIC ASSOCIATION OF NIGERIA


Quick Navigation


Niger J Paediatr 2016; 43 (4): 252 – 257
ORIGINAL
Onubogu UC
Implementation of Kangaroo
Okoh BA
mother care by health workers in
Nigeria
DOI:http://dx.doi.org/10.4314/njp.v43i4.4
Accepted: 4th August 2016
Abstract :
Background: Kangaroo
122(77.7%)
doctors
and
35
Mother Care (KMC) has been
(22.3%) nurses were studied. 84
Onubogu UC (
)
proven to significantly improve
(53.5%) practiced KMC. The rea-
Department of Paediatrics,
growth, reduce mortality and mor-
sons for not practicing KMC were
Braithwaite Memorial Specialist
Hospital, Port Harcourt, Rivers State.
bidity in low birth weight infants.
lack of policy reported by 43
Nigeria
The impact of KMC in newborn
(58.9%) and inadequate place for
Email: utchayonubogu@yahoo.co.uk
care is expected to be greatest in
the mothers to stay 30(41%).The
Africa due to limitations in health
level of practice was significantly
Okoh BA
care.
higher among respondents that
Department of Paediatrics,
Objective: The
aim of
this study
worked in facilities that care for
University of Port Harcourt Teaching
was to determine the proportion
sick neonates (p = 0.049), have
Hospital, Port Harcourt. Rivers State,
of
Nigerian health workers ren-
functional incubators (p = 0.014)
Nigeria
dering paediatric care who prac-
and practice KMC (p < 0.001).
tice KMC in their institution, and
Conclusion: Hospitals
should have
identify some challenges affecting
a
written KMC policy and provide
the practice of KMC in Nigerian
KMC wards in order to improve
health institutions.
implementation of KMC practice
Method: A
cross sectional
study
in
Nigeria.
of
the participants at 45 annual
th
scientific conference of the Paedi-
Keywords: Health
workers,
atric Association of Nigeria was
kangaroo mother care, low birth
conducted.
weight, neonate, Nigeria
Result: A
total of157
respondents
Introduction
located often in distant referral hospitals which are un-
derstaffed and ill-equipped. The implementation of
Kangaroo Mother Care (KMC) is the early, prolonged
KMC on an appreciable scale in the relatively few health
and
continuous skin – to – skin contact between the
facilities in low income countries is the only way this
mother (or substitute) and her low birth weight infant,
strategy can make significant impact in reducing the
both in hospital and after early discharge, until at least
unacceptably high neonatal mortality in these low in-
the 40th week of postnatal gestation age. The develop-
1
come countries.
ment of this method of care in early 1970s, was moti-
vated by problems arising from shortage of incubators,
In
Nigeria, it was estimated that KMC would save over
overcrowding and the impact of mother and newborn
19,000 lives by 2015 if all preterm neonates were to be
reached. For this to succeed, the health worker that ren-
5
separation in hospitals caring for low birth weight in-
fants.
1
ders pediatric care would have to start implementing
KMC in the health facility where they practice and then
KMC has been proven to significantly improve growth,
aim to scale it up to involve the grass roots. According
reduce mortality and morbidity particularly from hypo-
to
reports by Victora et al, one of the reasons attributed
thermia, hypoglycemia and nosocomial sepsis in neo-
to
poor expansion of KMC practice on a large scale in
nates with birth weight of <2000g. Lawn et al, in a
2,3
most low- and middle-income countries is because in
meta-analysis of three randomized control trial studies
these countries, KMC implementation started at a teach-
reported that KMC decreased mortality in neonates with
ing or other tertiary hospital without expanding to dis-
trict hospitals. Within the health facility, Provision of a
6
birth weight of <2000 g by 51%. More than three dec-
4
ades after its development, KMC is now recognized by
private comfortable environment and having written
global experts as an integral part of essential newborn
protocols has also been identified as one of the support-
ing factors that promote KMC practice.
6,7
care.
In
Nigeria
It
is expected that the impact of KMC in newborn care
KMC was first introduced in the late 1990s through a
would be greatest in Africa with a significant number of
resident pediatrician at the University of Lagos Teaching
low income countries. This is because of limited options
Hospital following a month-long training in Bogotá,
Colombia. KMC was also declared as the best option of
8
for care for preterm babies with few neonatal care units,
253
practice in 1998 during the 29 annual general and sci-
th
Respondents scoring less than 50% were considered to
entific conference of the paediatric association of Nige-
have
poor practice, those scoring 50 – 75% moderate,
ria.
More than 2 decades after the adoption of KMC in
[9]
and
those scoring above 75% as having good practice of
Nigeria, with various training programs organized by
KMC.
ministry of health and Non-governmental organizations
Data collected was entered and analyzed using EPI
at
different levels of heath care from tertiary to primary,
INFO version 7. Chi- squared test and Fishers Exact test
there has not been a study done to assess the level of
were used to test for significant associations between
adoption of this practice in health institutions in Nigeria.
proportions. Comparison of means was done with the
We
set out to determine the proportion of Nigerian
student’s t test. A p value of 0.05 or less was considered
health workers at a paediatric conference rendering pae-
statistically significant.
diatric care who practice KMC in their institution, and
identify some challenges affecting the practice of KMC
in
Nigerian health institutions.
Results
There were 157 respondents recruited in the study that
Methods
completed and returned questionnaires out of 223 ques-
tionnaires distributed giving a response rate of 70.4%.
th
A
cross sectional study of the participants at 45 annual
Of
this, 62 (39.5%) were males and 95 (60.5%) were
scientific conference of the Paediatric Association of
females giving a male to female ratio of 1: 1.5. Table 1
Nigeria held in Calabar, Nigeria in January 2014 was
shows the age group and gender distribution of the re-
conducted. The annual scientific meeting of the Pediat-
spondents.
ric Association of Nigeria is a forum that is usually at-
tended by health workers who are involved or have in-
Table 1: Age
group and
gender distribution
of respondents
terest in the care of children. Attendees are usually made
Gender
up
of doctors and nurses at different levels of their pro-
Male
Female
Total
fession practicing in and outside Nigeria. The forum is a
Age
group (years)
N
(%)
N
(%)
N
(%)
place for rubbing of minds, sharing of experiences and
solutions to problems confronting both child health spe-
<20
0
(0.0)
1
(100.0)
1
(0.6)
cialists and the Nigerian Child.
20
– 30
2
(20.0)
8
(80.0)
10
(6.4)
31
– 40
39
(50.6)
38
(49.4)
77
(49.0)
41
– 50
15
(31.2)
33
(68.8)
48
(30.6)
Nigeria is a country with 36 states divided into six geo-
51
– 60
5
(31.2)
11
(68.8)
16
(10.2)
political zones [North Central (Benue, FCT, Kogi,
>60
1
(20.0)
4
(80.0)
5
(3.2)
Kwara, Nasarawa, Niger and Plateau); North East
Total
62
(39.5)
95
(60.5)
157
(100.0)
(Adamawa, Bauchi, Borno, Gombe, Taraba and Yobe);
North West (Kaduna, Katsina, Kano, Kebbi, Sokoto and
The respondents consisted of health practitioners prac-
Jigawa); South East (Abia, Anambra, Ebonyi, Enugu
ticing in 26 out of the 36 states in Nigeria. Respondents
and Imo); South South (Akwa Ibom, Bayelsa, Cross-
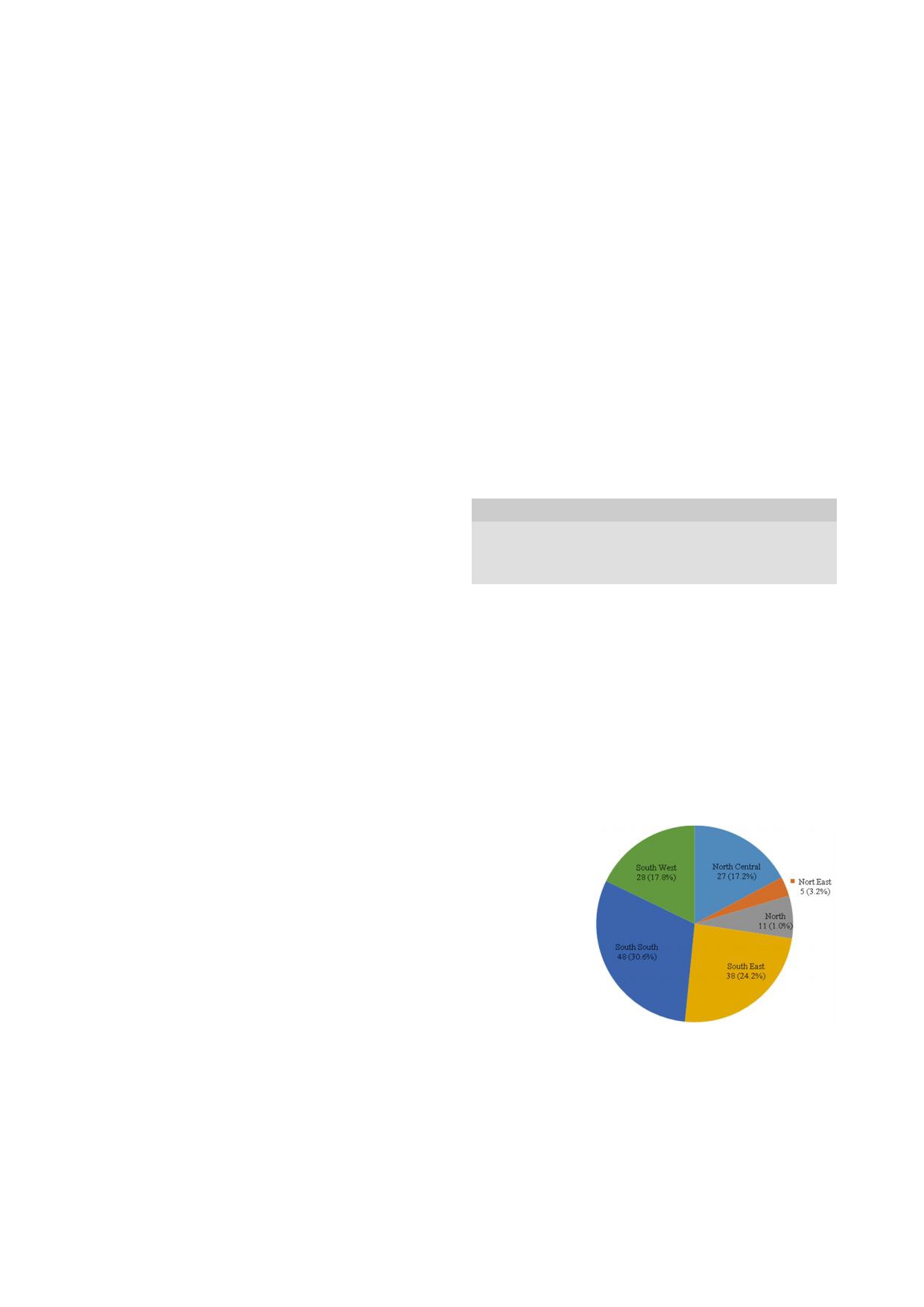
from the South – South geo – political zone were the
River, Delta, Edo and Rivers); and South West (Ekiti,
most, represented48 (30.6%) while those from the North
Lagos, Osun, Ondo, Ogun and Oyo]. This was used to
east had the least number of respondents 5 (3.2%)
categorize the location of the health facilities where the
(Figure 1).
participants practiced.
Fig 1: Distribution
Ethical clearance was obtained from the local organizing
of
respondent’s
committee of the conference. Verbal consent was ob-
health facilities by
geo
– political
tained from the attendees and questionnaires were given
zones of Nigeria
to
those that gave consent. The filled out questionnaires
were continually retrieved throughout the three days
duration of the conference. Information collected from
respondents included health facility information [name,
location, type of practice, level of care rendered, avail-
ability of neonatal care, transport incubators and ade-
quacy of incubators, and routine practice of KMC] and
Health worker information [age, gender, occupation,
level of qualification, area of specialty, years of practice,
Of
the 157 respondents, there were 122 (77.7%) doctors
personal practice experience in educating parents or
and 35 (22.3%) nurses. A total of 138 (87.9%) respon-
actual practice]. Questions on various levels of personal
dents worked in tertiary institutions and only one re-
practice of KMC by the respondents including prescrib-
spondent worked in a primary health care center. Major-
ing, teaching and giving information to parents, super-
ity of the respondents 97.3% had been practicing as
vising and assisting in provision of KMC to neonates
health care providers for more than 5 years (Table 2).
were asked in the questionnaire. Each positive answer
was scored one point and the total scores were added up.
254
Table 2: Qualification,
care level
and years
of practice
of
Table 4: Distribution
of health
workers that
practice KMC
by
Respondents
geo –
political zones
Frequency (N)
Percent (%)
Hospital Kangaroo Mother Care
Qualification
Consultant
59
37.6
practice
Senior Registrar
36
22.9
Yes
No
Total
P
Registrar
24
15.3
Geo
– political zone
N
(%)
N
(%)
N
Medical Officer
3
1.9
North Central
10
(37.0)
17
(63.0)
27
0.05
Nurse
35
22.3
North
East
0
(0.0)
5
(100.0)
5
0.02
Care level of health facility
North
West
9
(81.8)
2
(18.2)
11
0.05
Primary
1
0.6
South
East
21
(55.3)
17
(44.7)
38
0.80
Secondary
18
11.5
South South
28
(58.3)
20
(41.7)
48
0.42
Tertiary
138
87.9
South West
16
(57.1)
12
(42.9)
28
0.67
Years of practice
Total
84
(53.5)
73
(46.5)
157
<5
9
5.7
5-10
46
29.3
11-15
46
29.3
As
shown in Table 5, the level of practice of KMC
16
- 20
17
10.8
among respondents was significantly higher among
>20
39
24.9
respondents that worked in facilities that care for sick
neonates (p = 0.049), those that worked in facilities with
One hundred and four (98.1%) respondents worked in
functional incubators (p = 0.014) and those that worked
facilities that care for sick neonates and the facilities of
in
facilities that practice KMC (p < 0.001). The level of
84
(53.5%) of the respondents practiced Kangaroo
practice was also higher among females, nurses and re-
Mother Care (Table 3).
spondents that practiced in the Southern part of the
Country but the observed differences were not statisti-
Table 3: Some
neonatal care
practices of
facilities where
re-
spondents practice
cally significant. The level of practice tended to improve
with increasing years of practice except among those
Neonatal care practices of facility
Yes
N(%)
No
N (%)
that had practiced for 11 – 15 years where a slight
Care of sick newborns
154
(98.1)
3
(1.9)
decline was noted. It also tended to improve with
Availability of incubators
85
(54.1)
72
(45.9)
increasing care level of facility from Primary to Tertiary.
Availability of transport incubators
53
(33.8)
104
(66.2)
Practice of Kangaroo Mother Care
84
(53.5)
73
(46.5)
Table 5: Relationship
between level
of practice
of KMC
and
some variables
Of
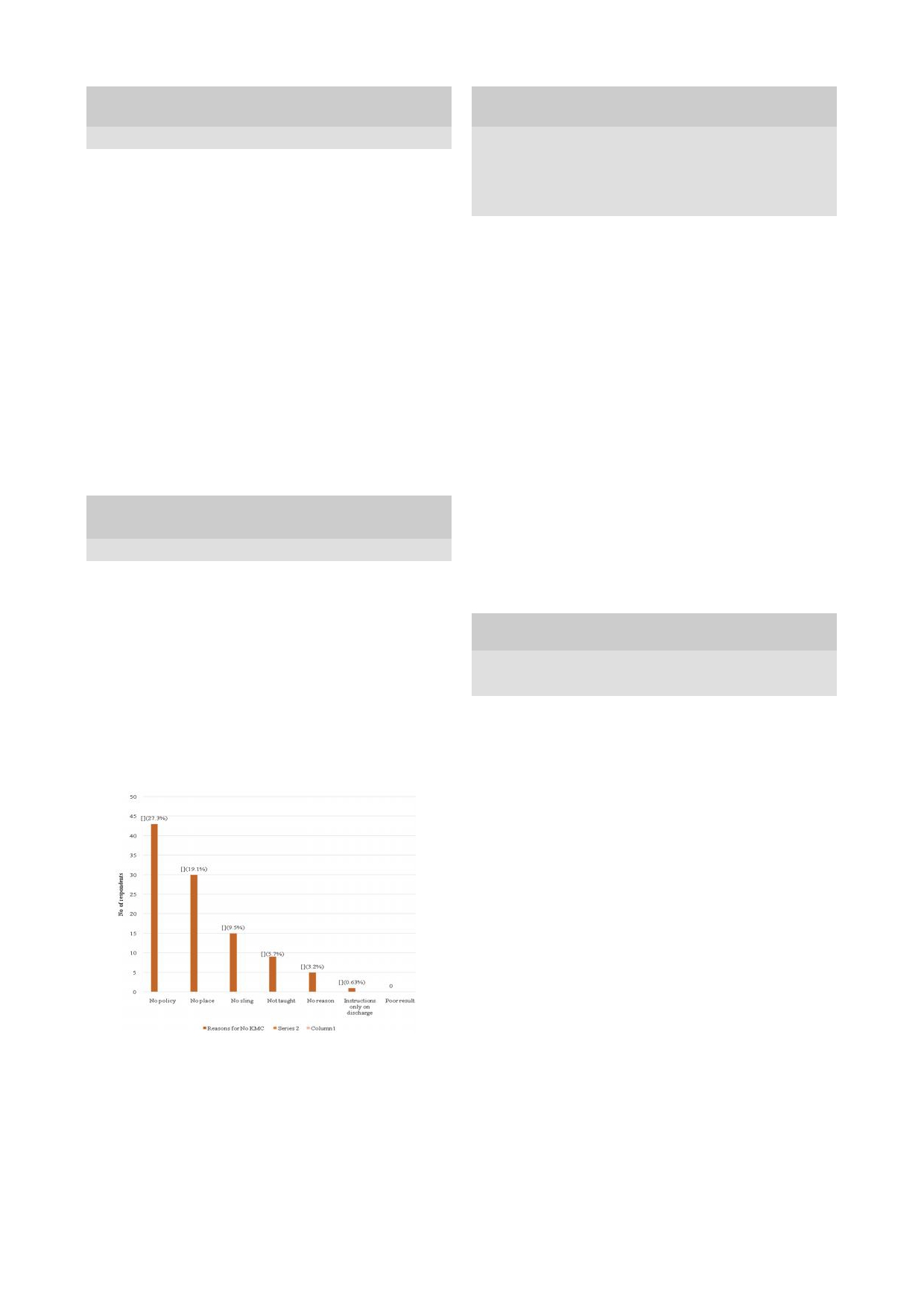
the 73 respondents that did not practice KMC in their
Level of
practice of KMC
facilities, the most common reason reported by 43
Moder-
Variable
Good
Total
P
(58.9%) was a lack of policy on the practice of KMC.
ate /
Poor
Gender
Male
34
(54.8)
28 (45
2)
62
(39.5)
0.084
No
respondent reported poor Result as a reason for not
Female
65
(68.4)
30
(31.6)
95
(60.5)
practicing KMC (Figure 2).
Occupation
Doctor
72
(59.0)
50
(41.0)
122
(77.7)
0.050
Nurse
27
(77.1)
8
(22.9)
35
(22.3)
Fig 2: Reasons
for not
practicing Kangaroo
Mother Care
in
Paediatri-
Specialty
70
(58.8)
49
(41.2)
119
(75.8)
0.052
facilities of respondents
cian
Non -
paediatri-
29
(76.3)
9
(23.7)
38
(24.2)
can
Neonatolo-
Subspecialty
16
(61.5)
10
(38.5)
26
(16.6)
0.860
gist
Non -
neonatolo-
83
(63.4)
48
(36.6)
131
(83.4)
gist
Location
of
26
(60.5)
17
(39.5)
43
(27.4)
0.679
health
facility
North
South
73
(64.0)
41
(36.0)
114
(72.6)
Care level
of
Primary
0
(0.0)
1
(100.0)
1
(0.6)
0.603
health
facility
Secondary
11
(61.1)
7
(38.9)
18
(11.5)
Tertiary
88
(63.8)
50
(36.2)
138
(87.9)
Care for
sick
Yes
99
(64.3)
55
(35.7)
154
(98.1)
0.049*
neonates
No
0
(0.0)
3
(100.0)
3
(1.9)
Availability
of
KMC was practiced most among health care facilities in
Yes
61
(71.8)
24
(28.2)
85
(54.1)
0.014*
incubators
the North West geopolitical zone (81.8%) and not at all
No
38
(52.8)
34
(47.2)
72
(45.9)
among represented facilities from the North East zone
Practice
of
<0.001
Yes
70
(83.3)
14
(16.7)
84
(53.5)
(Table 4).
KMC in
facility
*
No
29
(39.7)
44
(60.3)
73
(46.5)
Years
of
<5
4
(44.4)
5
(55.6)
9
(5.7)
practice
5 - 10
30
(65.2)
16
(34.8)
46
(29.3)
0.605
11 -
15
28
(60.9)
18
(39.1)
46
(29.3)
16 -
20
12
(70.6)
5
(29.4)
17
(10.8)
>20
25
(64.1)
14
(35.9)
39
(24.8)

255
Discussion
ter. If KMC knowledge is impacted to these primary
care centers then they can efficiently follow up the pre-
Health workers from the South South (SS) geopolitical
term infants and give support to mothers who continue
region were the most represented in our sample popula-
KMC at home. Another reason the practice needs to be
tion while the North East (NE) was the least represented.
scaled up to the peripheral centers is the absence of
The location of the conference in which the study was
transport incubators seen in 66.2% of the health centers
carried was in the SS region so this could account for its
that respondents come from which is made up of mostly
high representation. The NE however has been reported
tertiary centers. With the poor social amenities that are
to
have the lowest number of pediatricians in Nigeria
obtainable in low income countries, ambulance services
with >600,000 children per pediatrician ratio.
10
There
are almost non-existent and as such KMC is the safest,
has also been incidences of terror attacks in the past one
practical way to transport a low birth weight infant born
year in the NE region leading to displacements of people
in
a remote or peripheral health center that needs to be
inclusive of health workers. Most (87.9%) of the health
transferred to a tertiary center for specialized neonatal
workers in our study population were in tertiary centers,
care.
it
is not surprising as Ekure et al had earlier reported that
87.5% of pediatricians in Nigeria were in the tertiary
The most common reason reported for not implementing
institutions. This brings to light, the essential need for
10
KMC was not having a written protocol. Absence of
pediatricians practicing in theses tertiary centers to iden-
clear guidelines on KMC is a barrier to its implementa-
tion
12,13
tify and adopt the secondary and primary health centers
Written protocols help institutions standardize
within their locality in order to influence and impact
their practice, it enables the members of staff to be con-
positively on their practice. The pediatricians ought to
sistent at following procedures to achieve set goals with
work in the consciousness of the fact that, their responsi-
minimal errors. In the practice of KMC, having written
bility is not confined to the four walls of the tertiary
protocols would help standardize the decision of who
health facility in which they work but that it extends
qualifies for the care, where it should be carried out and
down to the grass root. This can be called "The triangu-
discharge procedure. Another factor affecting KMC
lar care” with the pediatrician in the tertiary facility at
practice in our study is not having a suitable environ-
the top of this triangle.
ment. For places where KMC has been successfully
practiced they had a dedicated KMC ward with beds for
the mothers
.3,14
In
our study 45.9% of the respondents did not have incu-
Most health facilities in low income
bators in their health facility and 66.2% did not have
countries barely have enough space for baby cots and
transport incubators. The needs that contributed to high
incubators and cannot provide a ward for stable mothers
neonatal mortality which inspired the introduction of
to
stay and practice KMC. Besides that, there is the
KMC in the early seventies is still with us, especially in
problem of transferred cost of such KMC ward occu-
low income countries and these include inadequate incu-
pancy on the family who already has the financial bur-
bators, overcrowding and the impact of mother and new-
den of a long stay preterm infant. If KMC wards are to
born separation in hospitals caring for low birth weight
be
provided, the problem of who to finance its mainte-
infants. Added to the afore mentioned, is the unavail-
1
nance would have to be addressed, at no added cost to
ability of transport incubators to transport preterm in-
the mothers practicing KMC within the hospital. In this
fants born in peripheral centers to bigger hospitals where
era of public-private partnership in Nigeria health indus-
neonatal care is available. All these highlights the need
try, KMC wards can be subsidized and charged at bi-
to
train primary health workers at the grass root on
weekly and monthly rates. Mothers that need to stay
KMC as this may be their only transportation practice
longer in KMC wards could also be given higher dis-
option for the low birth weight infant.
counts. This would, ease the financial burden on the
parents and also benefit the hospital, with improved in-
From our study only 53.5% of the health workers prac-
fant survival and patronage.
ticed KMC, considering that these health workers are
mostly from tertiary institutions and each tertiary institu-
Lack of training contributed as a reason for not imple-
tion is a referral center for other secondary and primary
menting KMC in only 9 (12.3%) of those not practicing
facilities within their regions. This apparently translates
KMC. This supports reports which states that in most
to
a large population of low birth weight infants being
low income countries training was done for most health
nursed without the benefits of KMC. Victora et al
workers in tertiary institutions where most of our re-
stressed the importance of achieving equity in KMC
spondents worked thus, accounting for the high number
of
respondents that had been trained in KMC.
6,14
delivery as groups that are left behind are often those
It
is
with the highest burden of morbidity and mortality. This
6
remarkable to note that no health worker reported that
can be said of the need for KMC which is high in the
they did not get any beneficial result from practicing
grass root and primary health care centers where most of
KMC. This could be because at this point, more than
the deliveries take place in low income countries. Stud-
four decades after development of KMC, the benefits of
ies have shown better weight gain among low birth
the practice is not in doubt among health workers. The
weight infants discharged home on KMC than those in
problem really is, implementation bottlenecks of a prac-
conventional care.
2,11
Follow up after discharge for
tice we are convinced is beneficial to children that need
LBW babies should be done in the health facility nearest
it. Another reason given for non-implementation of
to
the infant which is usually a primary health care cen-
KMC was lack of KMC support pouch. This is unfortu-
256
nate
as any soft piece of fabric, about a meter square,
facilities and community.
can
be used to support the baby on the mother’s chest
for KMC. Although, only 1% of health workers prac-
15
KMC like every clinical skill, improves with practice so
ticed KMC only on discharge, it is important to address
it
is not surprising that its level of practice was higher
the fact that this practice is not beneficial to the baby
among health workers that cared for sick neonates, those
and the institution as both parties would be short
that had functional incubators and those that were al-
changed from benefiting from the advantages of KMC
ready practicing KMC. The regular practice of KMC
early in the care of low birth weight infants. Commenc-
contributed to a relatively higher level of practice than
ing KMC only during discharge would also lead to poor
other health workers. KMC has been described as pri-
compliance rate on the part of the mother as they would
marily a nursing intervention with medical support and
not have had enough experience with KMC before being
Nurses have been described as the catalyst for KMC
implementation and practice. It is therefore not surpris-
16
discharged to continue at home.
ing
that in our study Nurses had higher level of practice
The
health workers from NW had the highest practice of
than
doctors, as they probably were more involved in the
KMC.
The reason for this may be due to the impact of
practice of KMC.
the training program embark upon by Partnership for
Reviving Routine Immunization in Northern Nigeria;
Maternal Newborn and Child Health Initiative, in which
over 260 health workers from 3 target states ( 2 in NW:
Conclusion
Katsina, Zamfara and 1 in NE :Yobe) were trained in
KMC with the mandate to implement and step down to
In
conclusion more than half of the Nigerian health
their individual states. The NW seemed to have made
8
workers that responded practiced KMC. The common
significant progress far exceeding the country’s average
reasons for not implementing KMC in our health facili-
KMC practice rate (53.5%). The NE however had the
ties were not having a written policy and not having an
lowest KMC practice rate without reflecting the benefits
adequate place for the mothers to stay.
of
the same program carried out in NW. The fact that the
We
recommend that hospitals should have a written
NE
has very few health workers as earlier stated could
KMC policy in order to successfully practice it. We also
account for its low KMC practice rate because, the im-
recommend provision of KMC wards in order to provide
plementation and stepping down of KMC at the state
a
suitable environment for the implementation of KMC
level requires health workers which the region is in short
in
our health facilities.
supply of. The overall KMC practice rate in Nigeria is
low, however, the significant progress recorded by the
Conflict of interest: None
PRRINN-MCH training program can be adopted on a
Funding: None
national level to improve KMC practice in our health
Reference
1.
Cattaneo A, Davanzo R, Uxa F.
5.
Kinney K, Lawn J, Kerber k and
8.
Aboda A, Williams A. An update
Recommendations for the Imple-
Save the Children US. Science in
technical brief: Saving Low Birth
mentation of Kangaroo Mother
Action; saving the lives of Africa’s
Weight Newborn Lives through
Care for Low Birth weight Infants.
mothers, newborns & children.
Kangaroo Mother Care (KMC)
ActaPaediatrica. 1998; 87:440 – 5.
Report. African Science Academy
PRRINN-MNCH Experience
2.
Rao
Suman PN, Udani R, Nanavati
Development Initiative.2009;1.
2012;1. Available at :http://
R.
Kangaroo mother care for low
Available at http://www.who.int/
www.prrinn-mnch.org/
birthweight infants: a randomized
pmnch/topics/continuum/
documents/KMC_UPDATE
controlled trial. Indian
Pediatr
scienceinaction.pdf Accessed fe-
March2012_14.pdf. Accessed
2008;45:17-23.
buary 3, 2016.
February 3,2016.
3.
Worku B, Kassie A. Kangaroo
6.
Victora CG, Rubens CE, and the
9 .
Ajayi AO. Improving neonatal
mother care: a randomized con-
GAPPS Review Group. Global
care in Nigeria using appropriate
trolled trial on effectiveness of
report on preterm birth and still-
technology. Guest lecture at the
29
Annual general and scientific
th
early kangaroo mother care for the
birth (4 of 7): delivery of interven-
low
birthweight infants in Addis
tions. BMC Pregnancy Childbirth.
conference of the paediatric asso-
Ababa, Ethiopia. J
Trop Pediatr
2010; 10 Suppl 1:S4.
ciation of Nigeria in Ilorin,
2005;51:93-7.
7.
Pattinson RC, Arsalo I, Bergh AM,
Kwara State, Feb 1998.
4.
Lawn JE, Mwansa-Kambafwile J,
Malan AF, Patrick M, Phillips N.
10. Ekure
EN, Esezobor
CI, Balogun
Horta BL, Barros FC, Cousens S.
Implementation of kangaroo
MR,
Woo JG, Mukhtar-Yola M,
Kangaroo mother care’ to prevent
mother care: a randomized con-
Ojo
OO et al. Paediatrician work-
neonatal deaths due to preterm
trolled trial of two outreach strate-
force in Nigeria and impact on
birth complications. Int.
J. Epide-
gies. Acta
Paediatr. 2005;94
child health: Niger
J Paediatr
miol. 2010;39Suppl 1: i144-i154.
(7):924-97.
2013; 40 (2): 112 – 118.

257
11.
Nguah BS, Wobil PNL, Obeng R,
13.
Seidman G, Unnikrishnan
15.
World Health Organisation. Kan-
Yakubu A, Kerber KJ, Lawn JE, et
S,
Kenny E, Myslinski S, Cairns-
garoo mother care: a practical
al
Perception and practice of Kan-
Smith S, Mulligan B, et alBarriers
guide. Geneva, Switzerland:
garoo Mother Care after discharge
and
enablers of kangaroo mother
Department of Reproductive
from hospital in Kumasi, Ghana: A
care practice: a systematic review.
Health and Research World
longitudinal study. BMC
Preg-
PLoS One 2015; 10(5).
Health Organization ; 2003.
nancy Childbirth. 2011; 11: 99.
14.
Solomons N, Rosant C. Knowl-
16.
Davy K, Van Rooyen E. The
12.
Bergh AM, Arsalo I, Malan AF,
edge and attitudes of nursing staff
neonatal nurse’s role in kangaroo
Patrick M, Pattinson RC, Phillips
and
mothers towards kangaroo
mother care. Prof
Nurs To-
N.
Measuring implementation
mother care in the eastern sub-
day.2011;15(3):32-37.
progress in kangaroo mother care.
district of Cape Town. S
Afr J
Clin
ActaPaediatr 2005;94:1102-8.
Nutr 2012;25(1):33 -39.







