

Copyright 2015 © Nigerian Journal of Paediatrics. All Rights Reserved. . Powered by Pelrox Technologies Ltd
ISSN 03 02 4660 AN OFFICIAL JOURNAL OF THE PAEDIATRIC ASSOCIATION OF NIGERIA


Quick Navigation

Niger J Paediatr 2016; 43 (4): 291 – 294
CASE
REPORT
Ekanem EE
Ulcerative colitis in a Nigerian
Ikobah JM
Ngim OE
child: case report
Okpara HC
DOI:http://dx.doi.org/10.4314/njp.v43i4.11
Accepted: 2nd June 2016
Abstract :
Ulcerative colitis
(UC)
diagnosis. An 11 year old Nigerian
is
a chronic re-occuring inflam-
male child who was referred to the
Ekanem EE
(
)
matory disease affecting mainly
University of Calabar Teaching
Ikobah JM, Ngim OE
the colon. It is more prevalent in
Hospital with bleeding per rectum,
Okpara HC
Department of Paediatrics,
the
United
Kingdom,
North
abdominal pain and swelling, bilat-
University of Calabar/University of
America Scandinavia and less
eral leg swelling and weight loss
Calabar Teaching Hospital, Calabar,
common in southern Europe, Asia
for seven months prior to presenta-
Cross River State, Nigeria
and Africa. Commonly, UC is
tion. Examination and investiga-
Email:
suspected in patients presenting
tions done including colonoscopy,
emmanuelekanem@unical.edu.ng
with bloody diarrhoea, tenesmus,
histology of biopsy, faecal calpro-
abdominal pain, and, when se-
tectin and pANCA confirmed ul-
vere, weight loss, fatigue, and
cerative colitis. Ulcerative colitis
vomiting. Perhaps one child so far
though rare in Africa may have
with UC has been reported south-
been missed in some children due
west geo-political zone of Nige-
to
mis-conception and lack of di-
ria. We here report the first case
agnostic facilities/expertise. We
of
ulcerative colitis in a child in
may begin to see more of this with
south-south Nigeria.
increasing interest in the sub-
The objective of this report was to
specialty of paediatric gastroen-
highlight the occurence of ulcera-
terology and presence of diagnos-
tive colitis in a Nigerian child in
tic facilities.
the
setting
of
poor
socio-
psychological/economic
back-
Key word: Ulcerative
Colitis,
ground coupled with difficulty in
Diagnostic difficulties, Nigerian
investigating patient to arrive at a
child
Introduction
tenesmus, abdominal pain, and, when symptoms become
severe, weight loss, fatigue, and vomiting. Children
Ulcerative colitis (UC) is a chronic re-occuring inflam-
have unique age-related considerations, such as growth,
matory condition of the colon, extending continuously
puberty, nutrition, and bone mineral density (BMD)
from the rectum proximally to a varying degree. Most
accretion during adolescence, as well as differing psy-
chosocial needs and development.
7,8
children with
ulcerative colitis present between the ages
of 10 and 18
years. The
incidence of
pediatric-onset
1,2
Ulcerative colitis is thought to be rare in sub-Saharan
UC, forms roughly 15% to 20% of patients of all ages
Africa, however, in Nigeria, ulcerative colitis has been
reported in adults.
9,10
with UC, ranging between 1 and 4 of 100,000/year in
It
was also reported in a seven year
Children
old female child in south-west Nigeria.
11
most North American and European regions.
1-3
We
report a
and adults develop
similar symptoms however children
confirmed case of ulcerative colitis in an 11 year old
often present with more
extensive disease. Childhood-
[4]
child in south-south Nigeria.
onset UC is extensive in 60% to 80% of all cases, twice
as
often as in adults with 82% of children at first pres-
4
Case report
entation have a pancolitis compared to 48% of adults.
5
The
extent of the disease is associated with disease se-
This
was an 11 year old adolescent male who presented
verity, therefore, most pediatric-onset UC have a worse
to
the University of Calabar Teaching Hospital, Calabar,
disease course. The pathogenesis of
ulcerative colitis is
6
Cross River State, Nigeria with history of bleeding per
unknown. A widely
accepted hypothesis suggests that,
rectum, abdominal pain, abdominal swelling and weight
in the genetically
susceptible individual, a combination
loss
of seven months duration. Patient’s stool was mixed
of host and environmental
factors lead to the initiation
with
fresh blood. Abdominal swelling was insidious in
and perpetuation of an
abnormal intestinal immune re-
onset and gradually increased over time. There was as-
sponse, resulting in
Ulcerative colitis. Typically, UC
is
sociated history of abdominal pain which was dull and
suspected in a patient presenting with bloody diarrhoea,
continuous in nature. There was a positive history of
292
vomiting and easy satiety. There was a positive history
ence of 5-6 RBC per hpf. Echo- cardiography result was
of
weight loss and fever. Leg swelling occurred at same
normal. Hepatitis B and C screening was negative and
time as abdominal swelling. There was history of dysp-
HIV test was also negative. Summary of findings of
noea on exertion, no orthopnoea or paroxysmal noctur-
abdominal ultrasound scan using a 3.5MHz curvilinear
nal dyspnoea. He was given herbal preparation as en-
probe includes mild enlarged and coarse looking liver
ema in a herbal home. He also received treatment from a
with caudate lobe enlargement, minimal ascites and
secondary health facility from where he was referred to
splenomegaly, gall bladder enlargement and increase in
the UCTH. Patient is the second child in a family of
wall thickness but no convincing evidence of portal hy-
two. Parents are separated and patient lives with the
pertension.
grandfather, a peasant farmer.
C
– reactive protein assay was within normal limit.
On
examination he was acute on chronically ill looking,
Liver biopsy was not done due to the deranged INR.
conscious, wasted, small for age, a febrile, severely pale,
Faecal calprotectin result was 155.57mg/kg faeces( bio-
jaundiced with bilateral pitting pedal oedema. Respira-
logical reference interval <25mg). Peri-nuclear anti neu-
tory
rate was 32cycles/minute, chest was clinically clear,
trophil cytoplasmic antibody (p-ANCA) was positive.
pulse
rate
was
88/minute,
blood
pressure
was
Upper and lower GI endoscopy was done and samples
I00/60mmHg, heart sound was SI and S2. Patient had a
taken for histology and cytology. Both the faecal calpro-
grossly distended abdomen with tenderness over the
tectin and p-ANCA assay were done in India as we
right and left hypochondria, liver was enlarged by 8cm
could not find a local laboratory that could perform the
below the right costal margin firm, tender, nodular, with
test. Upper GI endoscopic findings were normal with no
poorly defined edge. The spleen was 6cm enlarged be-
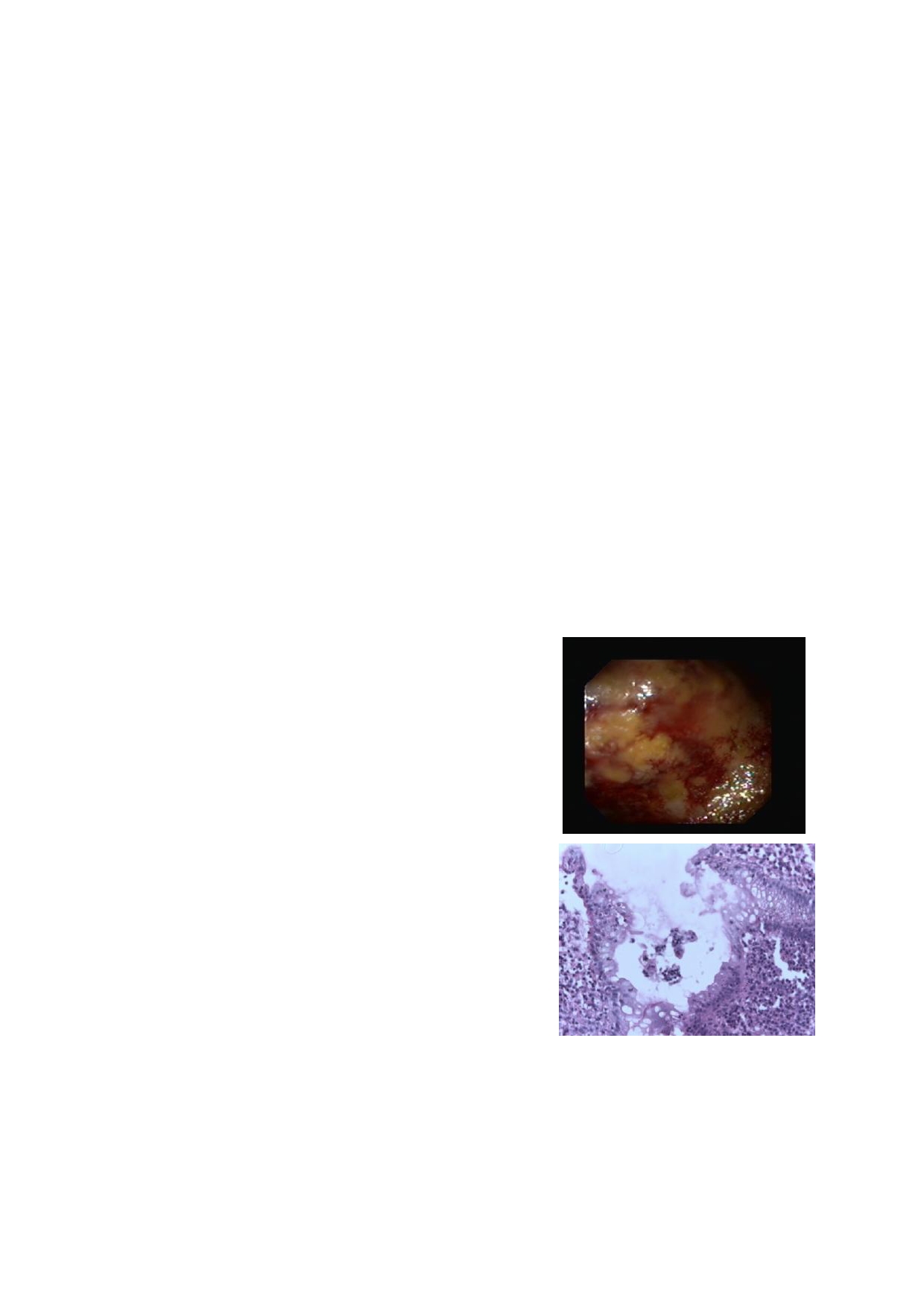
evidence of varices. Colonoscopy showed extensive
low the left costal margin, firm, smooth, non tender.
haemorrhagic mucosa of the large bowel all the way to
Fluid thrill was demonstrable. Rectal examination re-
the transverse colon (Fig. 1). Lesions were worse in the
vealed good anal hygiene, anal tags present at 4 o’
rectosigmoid
area. No ulcers, polyps, diverticular or
clock, 7 o’clock and 11 o’clock positions, normal
tumour were seen and no haemorrhoids . Cytology was
sphincteric tone, no palpable rectal masses. Examining
negative for malignancy and histology result showed
finger stained with feaces mixed with blood. An initial
chronic non-specific cololitis (Fig. 2). The activity of
diagnosis of chronic liver disease was made.
UC
using the paediatric ulcerative colitis activity index
(PUCAI) for the index patient was a score of 45 giving
him a moderate disease at diagnosis.
Results
Fig 1
Packed cell volume ranged between eight percent and
19%, patient was transfused four times while on admis-
sion. Full blood count showed total white cell count of
5.8%, erythrocyte sedimentation rate of 55mm/hr
(Westergren method), neutrophil of 67%, lymphocyte of
33%,
evidence of aniscocytosis, microcytosis, hy-
pochromasia and poikilocytosis. Liver function test done
showed total bilirubin of 58umol/l (normal range of 0.0-
17.0 ), direct bilirubin of 45.5umol/ (normal range of 0.0
-6.8 ), indirect bilirubin of 12.8umol/l (normal range of
0.0-10.3), alanine aminotransferase/SGPT of 41.0U/L
(normal range of 0-40 ), aspartate transferase/SGOT of
Fig 2
80.0U/L (normal range of 0-37 ), alkaline phosphatase
of
753U/L (normal range of 245-770), total protein of
57g/L(normal range of 55.0-82.0 ), albumin of 34g/L
(normal range 37.0-53.0 ), globulin of 23g/L (normal
range 15.0-36.0), GGTP 243.4U/L (normal range 10.0-
71.0). C-reactive protein level was within normal limit.
Lipid profile showed total cholesterol 3.6mmol/l
(normal range 3.6-5.2), HDL Cholesterol 1.6mmol/l
(normal range of 0.9-1.5), LDL Cholesterol 0.7mmol/l
(normal range of 1.9-3.5), triglyceride 2.9mmol/l
(normal range of 0.6-1.7). Initial prothrombin time was
30.5 seconds (prothrombin control 15 second), interna-
Discussion
tional normalized ratio (INR) of 2.13. A repeat done
after vitamin K administration showed prothrombin time
UC
is known to occur globally though less common in
was 23.6 second (prothrombin control 15 second), inter-
Africa and especially sub-Saharan Africa. This could be
national normalized ratio of 1.65. Stool microscopy,
due to lack of diagnostic expertise and the fact that there
culture and sensitivity result was normal except for pres-
is
still a high burden of infective diseases to battle with
293
and
the thought of UC commonly seen as a westernized
Presently, there is no permanent medical cure for UC.
illness is far from it. However, with increasing interest
The general goals of treatment in children are to control
in
gastroenterology as a sub-specialization and improv-
symptoms of the disease with minimal adverse effects of
ing expertise, few cases has been reported in adults in
the medicines used and to achieve normal functioning of
13
Uganda.
14
Ghana South Africa,
12
Nigeria
9,10
UC
has
the
patient. The intensity of treatment is dependent on
also
been reported in a seven year old Nigerian child
the
severity of the disease. Patients with moderate ul-
but
without the current diagnostic investigations of en-
cerative colitis are usually treated on an outpatient basis.
doscopy, faecal calprotectin and P-ANCA to confirm
However our patient was admitted on account of severe
this
hence our patient is the first confirmed case of UC
anaemia, poor socio-economic background and dysfunc-
in
a paediatric patient in Nigeria.
11
tional home setting. After initial stabilization, he was
started on pediatric medical regimen with low residue
As
in other reported cases in Africa, the diagnosis of UC
diet and prednisolone. Two days into commencement of
in
our index patient was not thought of initially at first
therapy, blood in stool stopped, appetite improved and
presentation. Patient was treated for dysentery and with
patient became more ambulatory. However compliance
persistence of passage of bloody diarrhoea, deranged
to
medication was poor due to the dysfunctional home
liver function test and the need for recurrent blood trans-
setting. This was also reported as affecting treatment
success in the first reported case in Nigeria
11
fusion, patient had a colonoscopy with biopsy done and
UC
was confirmed. This therefore underscores the need
for a high index of suspicion even in African children
Patient has been lost to follow-up despite repeated
with chronic bloody diarrhoea, weight loss and recurrent
phone calls. This is commonly the case in patients with
anaemia. Cabrera-Abreu showed a diagnostic sensitiv-
14
chronic illnesses and even worse in children who have
ity and specificity of 90.8% and 80% respectively in
to
rely on adult caregiver. This has been reported in Ni-
gerian adults
9,10
patients with signs suggestive of IBD and existence of
with UC and in the Nigerian child with
UC. Late presentation to hospital is a major problem in
11
anaemia or thrombocytosis. In children with UC, blood
loss could occur in 84%, diarrhoea in 74% and abdomi-
sub-Saharan Africa. Patients patronize alternative medi-
nal pain in 62% of patients. Weight loss is less com-
15
cal practitioners as was the case in our patient before
mon in UC (35%) than CD (58%).
15
Our patient pre-
presenting to the hospital as a last resort. Delay or fail-
sented with all these symptoms. Extra-intestinal mani-
ure of diagnosis of IBD may also result from lack of
festations of IBD may be present in 25% to 35% of
awareness, denial of the presence of IBD by our physi-
children.
15
Our patient presented with perianal disease
cians and limited facilities for most of the key investiga-
(skin tags) and hepatic disease. Hepatic
abnormalities in
tions in our environment.
18-20
Paediatric endoscopy only
started recently in Nigeria.
19,20
children with
ulcerative colitis have been well de-
Perhaps with increasing
scribed.
16
While these are
typically identified after the
use of endoscopic diagnostic facilities, more cases of
ulcerative colitis
diagnosis, they may also precede the
IBD in children will be discovered.
gastrointestinal
symptoms.
16
Transient elevations
of
alanine
aminotransferase (ALT) occur in 12% of chil-
dren with ulcerative
colitis and appear to be related to
medications or disease
activity. Persistent ALT eleva-
Conclusion
tions suggest the
presence of primary sclerosing
cholangitis (PSC) or
autoimmune chronic hepatitis.
17
Ulcerative colitis is reported in a sub-Saharan African
Among children with
ulcerative colitis, 3.5% develop
child. Though this appears rare, mis-diagnosis and mis-
sclerosing cholangitis
and less than one percent develop
conception of its rarity in African children may have
chronic hepatitis. The
diagnosis of PSC may be sus-
accounted for lack of reports on this inflammatory dis-
pected based on
symptoms of chronic fatigue, anorexia,
ease in Africa.
pruritus or jaundice,
although many children may be
asymptomatic. The
diagnosis of PSC may be established
through a combination
of cholangiography and liver
Conflict of interest: None
biopsy. Our patient
could not have a liver biopsy done
17
Funding: None
due to deranged INR and
cholangiograpghy was far
reached.
Reference
1.
Mendeloff AI, Calkins BM. The
2.
Benchimol EI, Fortinsky KJ, Goz-
3.
Chong SK, Blackshaw AJ,
epidemiology of idiopathic inflam-
dyra P, Meta Van den Heuvel,
Morson BC, Williams CB,
matory bowel disease. In Kirsner
Johan Van Limbergen, Griffiths
Walker-Smith JA. Prospective
JB,
Shorter RG, eds. Inflamma-
AM.
Epidemiology of pediatric
study of colitis in infancy and
tory Bowel Disease.
Philadelphia:
inflammatory bowel disease: a
early childhood. J
PediatrGastro-
Lea &Febiger, 1988: 3 – 34.
systematic review of international
enterolNutr1986; 5(3): 352 – 358.
trends. Inflamm
Bowel Dis
2011;
4.
Gryboski JD. Ulcerative colitis in
17:423 – 439.
children 10 years old or younger.
J PediatrGastroenterolNutr1993;
17: 24 – 31.
294
5.
Mamula P, Telega GW, Markowitz
11.
Senbanjo IO, Oshikoya KA, On-
17.
Roberts EA. Primary sclerosing
JE,
Brown KA, Russo PA, Piccoli
yekwere CA, Abdulkareem FB,
cholangitis in children. J
Gastro-
DA
et al. Inflammatory bowel
Njokanma OF. Ulcerative colitis
enterolHepatol1999; 14: 588 –
disease
in children 5 years of age
in
a Nigerian girl: A case report.
593.
and
younger. Am
J Gastroen-
BMC
Research Notes 2012 5:564.
18.
Ekwunife CN, Nweke IG, Achusi
terol2002 Aug; 97(8): 2005 – 2010
12.
Nkrumah KN. Inflammatory Bowel
IB,
Ekwunife CU. Ulcerative
6.
Langholz E, Munkholm P, Krasil-
Disease at the Korle Bu Teaching
colitis prone to delayed diagnosis
nikoff PA, Binder V. Inflammatory
Hospital, Accra. Ghana
Med J.
in
a Nigerian population: Case
bowel diseases with onset in child-
2008 Mar;42(1):38-41
series. Ann
Med Health
Sci Res.
hood. Clinical features, morbidity,
13.
Segal I, Tim LO, Hamilton DG,
2015 Jul-Aug; 5(4):311-313
and
mortality in a regional cohort.
Walker AR. The rarity of ulcera-
19.
Ngim OE, Ikobah JM, Ukpabio I,
Scand J Gastroenterol1997 Feb;
tive colitis in South African blacks.
Bassey GE, Ekanem EE. Paediat-
32(2): 139 – 147.
Am J Gastroenterol. 1980 Oct; 74
ric
Endoscopy in Calabar, an
7.
Van
Limbergen J, Russell RK,
(4):332-336
emerging trend-Challenges and
Drummond HE, Aldhous MC,
14.
Billinghurst JR, Welchman JM.
prospects: A report of two cases.
Round
NK, Nimmo ER et al. Defi-
Idiopathic ulcerative colitis in
IOSR J.
Dental and
Medical
nition of phenotypic characteristics
African: a report of four cases.
Sciences. 2014 ;13(1):28-30
of
childhood-onset inflammatory
Brit.med.J. 1966;1:211-213
20.
Ikobah JM, Ngim OE, Adeniyi F,
bowel disease .
Gastroenterol 2008
15.
Sandhu Bk, Fell JME, Beattle RM,
Ekanem EE, Abiodun P. Paediat-
Oct; 135(4): 1114-22
Mitton SG. BSPGHAN Guidelines
ric
Endoscopy in Nigeria-humble
8 .
Fiocchi C. Inflammatory bowel
for
the management of inflamma-
beginning. Nig
J Paed.
2015;42
disease: etiology and pathogenesis.
tory bowel disease in children in
(2):147-150
Gastroenterol1998; 115: 182 – 205.
the
United Kingdom. 2008 Oct pp
9.
Ukwenya AY, Ahmed A, Odigie
1-36.
VI,
Mohammed A. Inflammatory
16.
Hyams J, Markowitz J, Treem W.
bowel disease in Nigerians: Still a
Characterization of hepatic abnor-
rare diagnosis? Annals
of Afr
Med
malities in children with inflamma-
2011; 10( 2):175-179
tory bowel disease. Inflamm
Bowel
10.
Alatishe OI, Otegbayo JA, Nwosu
Dis1995; 1: 27.
MN,
Lawal OO, Ola SO, Anyanwu
NC
et al. Characteristics of inflam-
matory bowel disease in three
tertiary health centres in sothern
Nigeria. West
Afr J
Med.2012 Jan-
Mar;31(1):28-31







