

Copyright 2015 © Nigerian Journal of Paediatrics. All Rights Reserved. . Powered by Pelrox Technologies Ltd
ISSN 03 02 4660 AN OFFICIAL JOURNAL OF THE PAEDIATRIC ASSOCIATION OF NIGERIA


Quick Navigation

Niger J Paediatr 2017; 44 (1): 39 – 41
CASE
REPORT
Fatungase OM
Usefulness of peripheral nerve block
Ogundipe AA
Adebanjo AA
as an aneasthetic technique in a criti-
cally ill Child – A case report
DOI:http://dx.doi.org/10.4314/njp.v44i1.8
Accepted: 6th December 2016
Abstract :
Regional anaesthesia in
regional anaesthesia. This case is
children is a growing field of in-
reported to highlight the prospect
Fatungase OM
(
)
terest in current anaesthesia prac-
of
regional anaesthesia for criti-
Ogundipe AA
tice. We report a case of brachial
cally ill children who require sur-
Department of Anaesthesia,
Olabisi Onabanjo University,
plexus block for a child with se-
gical interventions in resource-
Email: mamafat40@gmail.com
vere forearm necrotizing fasciitis
poor settings.
and
septicaemia. The need to
Adebanjo AA
avoid the multiple shortcomings
Keywords: brachial
plexus block,
Department of surgery,
of
general anaesthesia in a criti-
children, critical illness, septicae-
Olabisi Onabanjo University,
cally ill child prompted the use of
mia, regional anaesthesia
Ago-iwoye.
Introduction
in
a sick child who is not suitable for general anaesthe-
sia.
The growing use of regional anaesthesia in infants, chil-
dren and adolescents has increased the popularity of
Case report
peripheral nerve blocks (PNB) in children. PNB is a
Presentation, admission and treatment
form
of regional anaesthesia which is accomplished by
injecting a local anaesthetic near a nerve/nerves that
A 9
year old presented in the children emergency ward
controls sensation and movement to a specific part of
of
Olabisi Onabanjo University Teaching Hospital, Sa-
the
body. This causes temporary numbness in the area.
1
gamu, Nigeria on referral from a private hospital where
The growing use of the technique is a result of the in-
he
had presented with a 6 day history of fever, body
creased confidence of anaesthetists in performing pe-
pains and general malaise. He was admitted at the pri-
ripheral nerve blocks. PNB are typically used for surger-
vate hospital and given intravenous medications through
ies of the upper and lower extremities, also for some
the dorsum of the left arm. After three days the left arm
procedures around the neck and groin.
subsequently became swollen, tender with limitations of
Peripheral regional anaesthesia is of great utility in chil-
active movements, with blister formation. These, cou-
dren undergoing surgeries of the upper extremities. In
pled with the persistence of the symptoms necessitated
contrast to general anaesthesia, it avoids airway instru-
his referral to the teaching hospital.
mentation and the use of many drugs. The peculiarities
1,
of
this technique include the meticulous attention to dos-
On
admission he was acutely ill looking, pale and febrile
ing
as a result of the poor development of connective
(39ºC). He was in respiratory distress, tachypneic,
tissues and the likelihood of extensive spread of locally
tachycardic with a tender hepatomegaly. The left arm
administered drugs. Other important considerations in-
was
swollen, tender with coalescing blisters, necrotic
clude the risk of rapid absorption with attendant sys-
eschar and copious purulent exudates. The packed cell
temic toxicity, reduced duration of action and age-
volume was 15% and chest x-ray showed evidence of
related anatomic variations.
pulmonary oedema. generalized widespread fluffy exu-
dates. A diagnosis of septicaemia with focus in necrotiz-
The use of ultrasound guidance during axillary approach
ing fasciitis of the left upper limb, severe anaemia and
to
brachial plexus blockade allows for real-time visuali-
congestive cardiac failure was made. He was resusci-
zaion of anatomical structures; however some anaesthe-
tated, commenced on parenteral antibiotics, diuretics,
tists prefer nerve stimulation to guide peripheral block-
digitalis and blood transfusion. Bacteriological culture
ade, while some use both methods for greater accuracy
of
pus aspirate yielded Proteus sp. He was planned for
and
safety. However, the use of ultrasound scan and / or
extensive wound debridement three days after admission
peripheral nerve stimulator is subject to availability. Our
to
remove focus of sepsis.
centre does not have the capacity for either. Complica-
tions of axillary approach include infection at the punc-
Pre-anaesthesia Review
ture
site, axillary tenderness, heamatoma, intravascular
injection and nerve damage . This case report is to enu-
1,2
When
he was reviewed on the morning of surgery he
merate the prospects of blind axillary approach to pe-
was
still having temperature spikes despite intravenous
ripheral brachial nerve block, in a low-resource setting,
antibiotics. Urinary output was adequate. There were no
40
known allergies. He had been on nil per oris for 12
hours. He was mildly pale and weighed 28kg which was
Fig 3: Blockage
of the
appropriate for age. The respiratory and heart rates,
musculo-cutaneous
blood pressure and precordial activities were normal.
nerve.
Airway assessment for ease of intubation and mask ven-
tilation showed no abnormality. He had Mallampati 2
class with adequate mouth opening.
Abdominal examination revealed minimal ascites and
hepatomegaly of 4cm below costal margin. The left el-
bow was in gauze and bandaged dressing. The initial
laboratory findings included PCV 30%, negative retrovi-
ral screening, normal haemoglobin genotype and INR of
The debridement lasted 15minutes, with an estimated
1.0.
blood loss of 50mls. He had 100mls of 4.3% dextrose in
Assessment was resolving septicaemia, resolving con-
5th saline. The pulse rate ranged between 120 and 135
gestive cardiac failure. An American Society of Anaes-
beat per minutes during the procedure. There were no
thesiologist (ASA) physical status class assessment of
critical incidences or complications intra-operatively
IIIE was made.
Post operatively the arm was put in a POP back slab for
The mother consented to the use of peripheral nerve
support, and patient was transferred to the recovery
block with sedation following adequate patient informa-
room and later back to the ward. He made full recovery
tion.
and was discharged a month later.
Procedure In theatre
The child was placed supine. Pulse oximeter and pre-
Discussion
cordial stethoscope and Non- Invasive Blood Pressure
(NIBP) measurement apparatus were attached. Baseline
Although the clinical diagnosis of septicaemia was bac-
parameters were; PR 107bpm, Bp 106/67mmHg, SpO2
teriologically confirmed, it was unresolved whether cel-
was 97% at room air.
lulitis of the arm resulted to septicaemia or the reverse
He
was pre-medicated with IV hydrocortisone 100mg,
occurred. The cellulitis could also have been due to drug
sedated with IV 2.5mg midazolam with IV Paracetamol
-induced tissue injury with subsequent bacterial coloni-
50mg for analgesia. The injectate for the nerve block
zation. However the removal of pus and eschar in this
patient was essential for infection control. Anaesthetists
3
was made by mixing 5mls of 0.5% plain bupivacaine,
plus 10mls of lignocaine in adrenaline and 10mls of
are involved in the care of septic patients for resuscita-
sterile water.
tion, intensive care and anaesthesia for infection source
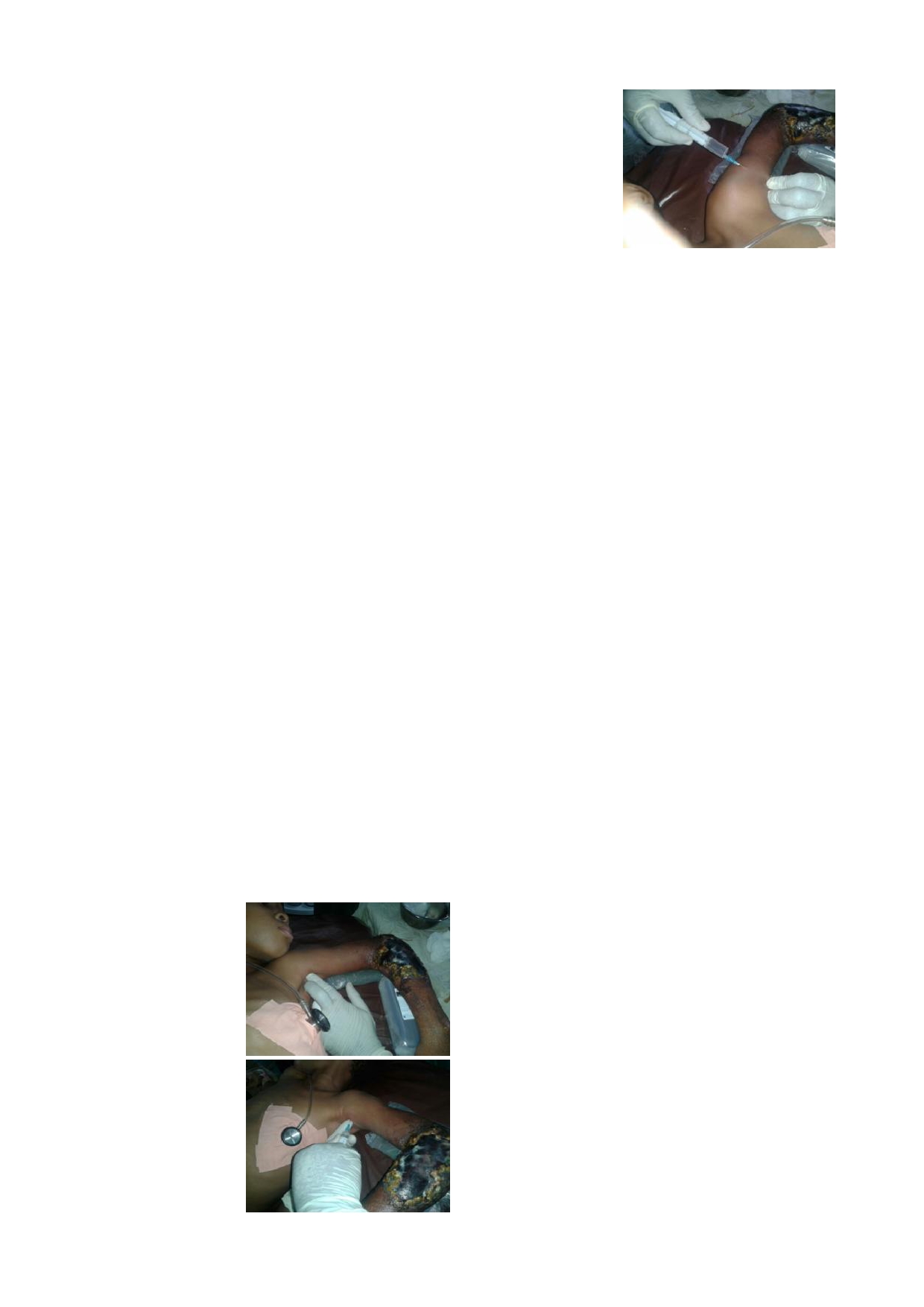
A
22G hypodermic needle, first made blunt by passing it
control. The latter includes drainage of abscess, debride-
through the sterile plastic sheath, was used for the axil-
ment of necrotic tissue, removal of infected devices and
lary block. The patient’s arm was abducted to 90 de-
foreign
bodies. The anaesthesia of septicaemic patient
grees (Fig 1) and the palpation method was used to iden-
for infection source control poses some challenges be-
tify the axillary artery. Skin infiltration was done with
cause of the gross heamodynamic instability and these
plain lidocaine. Test aspirate was done and 20mls of the
risks are higher in children.
injectate was used for the axillary block and 5mls for the
blockage of the musculocutanoeus nerve (Fig 2 and 3).
The available anaesthetic technique options include gen-
Efficacy was confirmed with loss of pain to surgical
eral anaesthesia or a brachial plexus block. The advan-
stimulation after 10 minutes. Supplemental 100% oxy-
tages of the use of regional anaesthesia as opposed to
gen was administered by face mask at 6l/minute flow
general anaesthesia include avoidance of the airway,
rate.
reduced postoperative nausea and vomiting, improved
tissue perfusion during re-implantations and the ability
Fig 1: Palpation
method
to
provide a continuous technique for repeated proce-
dures, and early hospital discharge. Brachial plexus
4
of
locating the axillary
artery prior to anaesthes-
block was chosen in this case because a full general an-
tic
infiltration
aesthesia will lead to administration of anaesthetic
agents that may further depress the myocardium thus
worsening the heart failure. It is also important to avoid
the
airway and the chest due to the accompanying pul-
monary oedema. Peripheral nerve blocks in septic pa-
tients cause less haemodynamic instability and less im-
munosuppression but also carry the risk of nerve dam-
Fig 2: Injection
of local
age,
allergic reaction, intravascular injection and risk of
anaesthetic into the axil-
toxicity. The index case had none of these complica-
3
lary sheath
tions.
Various approaches can be used for the brachial plexus
block; interscalene, supraclavicular, infraclavicular and
41
axillary approaches. Axillary approach is the common-
nes
and short acting opioids are useful in this regard.
est,
easiest and safest approach in all age groups espe-
Midazolam, a short acting benzodiazepine was used in
cially if it is done under the palpation method alone.
1,2,5
the
index case. It provided sedation, hypnosis and an-
The
continuous axillary block variant involves inserting
terograde amnesia without compromising the airway or
a
peripheral block catheter in the perineural space for
the
cardiovascular status of the patient. Paracetamol was
intermittent injections of the local anaesthetic solutions.
used
for pre-emptive analgesia after the effect of the
This
improves outcomes after microvascular sur-
nerve block must have worn off. This also avoided the
gery. Another safe method is the lateral infraclavicular
5
respiratory depressant effect of opioids.
approach which reduces the risk of pneumothorax . The
2
latter method is new in children, but gives a wider de-
gree of blockage, and can be done with the patient’s arm
at
the sides thus minimizing pain. Both can be made
Conclusion
safer and easier with the use of peripheral nerve stimula-
tor and / or ultrasound scan.
6,7.
Unfortunately, in low
The
case highlights the usefulness of peripheral nerve
resource centres where peripheral nerve stimulator and
block, in a septic peadiatric patient undergoing infection
an
ultrasound are not routinely available, the blind tech-
source control surgery. It is a viable option to consider
nique by palpation becomes extremely useful and handy.
when the patient is unstable for general anaesthesia. It is
safe, cost friendly and effective.
There are no published studies comparing general anaes-
thesia to upper limb regional anaestheisa . There are also
1
none comparing general anaesthesia with or without
Conflict of interest: None
upper limb blockade. Performing a nerve block in chil-
Funding: None
dren usually requires the use of sedation. Benzodiazepi-
Reference
1.
Mannion S. Regional anaesthesia
5.
Santhanam S, Amod S, Melanie K.
7.
Rukewe A, Fatiregun A, Arikawe
for
upper limb trauma: a review.
Common Peripheral Nerve blocks
OPA, Alonge TO. Brachial
Rom J Anesth Int care 2013; 20
in
Peadiatric Patients. Anesthesiol-
Plexus Blocks for Upper Extrem-
(1): 49-49.
ogy
News 2010: 19-26. Available
ity
Surgeries in a Nigerian Hospi-
2.
Fleischmann E, Marhofer P, Grehr
at
anesthesiologynews.com ac-
tal. E Afr
Med J
2011; 88(4):
135
cessed 18 September 2016.
th
M,
Walti B, Sitzwohl C, Kapral S.
-137.
Brachial plexus anaesthesia in
6.
Santhanam S, Lauren J. Taylor and
children: lateral infraclavicularvs
Amar S. M (2011). Ultrasound
axillary approach. Pediatric An-
Imaging for Pediatric Anesthesia:
aesth. 2003; 13(2): 103-108
A
Review, Ultrasound Imaging,
3.
Eissa D, Carton E. G. and D. J.
Mr
Masayuki Tanabe (Ed.), ISBN:
Buggy. Anaesthetic management
978-953-307-239-5, InTech,
of
patients with severe sepsis. Br J
Available from: http://
Anaesth 2010;105 (6): 734-4.
www.intechopen.com/books/
4.
Obasuyi BI, Alagbe-Briggs OT,
ultrasound-imaging/ultrasound-
Echem RC. Choice of anaesthesia
imaging-for-pediatricanesthesia-a-
for
Orthopaedic surgeries in a
review
developing country: How
appro-
priate? JMMS 2013; 4(3): 101-
106.







