

Copyright 2015 © Nigerian Journal of Paediatrics. All Rights Reserved. . Powered by Pelrox Technologies Ltd
ISSN 03 02 4660 AN OFFICIAL JOURNAL OF THE PAEDIATRIC ASSOCIATION OF NIGERIA


Quick Navigation

Niger J Paediatr 2016; 43 (4): 273 – 280
ORIGINAL
Kuti BP
Prevalence and predictors of
Adetola HH
Aladekomo TA
hypoxaemia in hospitalised
Kuti DK
children at the emergency unit of
a resource constrained centre
DOI:http://dx.doi.org/10.4314/njp.v43i4.8
Accepted: 23rd August 2016
Abstract :
Background: Hypoxae-
features. Eighty three (20.6%)
mia is often poorly detected and
were hypoxaemic including 40
Kuti BP (
)
treated in emergently-ill children
(38.1%) of those with respiratory
Aladekomo TA
in
resource-poor centres because
features at admission. Infancy,
Department of Paediatrics and
of
the non-availability of pulse
chest in-drawing, cyanosis and
Child Health
oximeters and similar facilities to
grunting were associated with hy-
Obafemi Awolowo University,
detect it. This study sets out to
poxaemia (p < 0.05) among those
Ile-Ife, Nigeria
determine the prevalence and sim-
with respiratory features, while
Email: kutitherapy@yahoo.com
ple predictors of hypoxaemia
infancy, pallor and tachycardia
among children with or without
were significant among those with
Adetola HH, Kuti DK
respiratory features at the emer-
no
respiratory features. Grunting
Department of Paediatrics,
gency unit of the Wesley Guild
(OR = 7.875; 95% CI=1.029-
Wesley Guild Hospital, Ilesa,
Hospital, Ilesa, Nigeria
15.797; p = 0.045) and Cyanosis
Nigeria
Methods:
Children aged one
(OR =13.579; 95% CI = 1.360-
month to 14 years were consecu-
14.379; p = 0.009) independently
tively recruited and prospectively
predict hypoxaemia among the
studied over an eight month pe-
children with respiratory features.
riod. All the children had their
Conclusion: Hypoxaemia
occurred
peripheral
oxygen
saturation
in
approximately one out of five ill
(SpO 2 ) measured at
presentation
children admitted to the emer-
using a portable pulse oximeter
gency unit of the WGH, Ilesa and
(Nellcor
(R)
N-200, USA) and hy-
was significantly associated with
poxaemia was defined as SpO 2
<
mortality. Emergently ill children
90%. Relevant history and exami-
with
cyanosis and grunting espe-
nation findings were compared
cially infants should preferentially
among hypoxaemic and non-
be
placed on oxygen therapy even
hypoxaemic children. Multivari-
when hypoxaemia cannot be con-
ate
analysis was used to predict
firmed.
the
presence of hypoxaemia.
Results: Four
hundred and
two
Key words :
Emergently ill
chil-
children were recruited with male
dren, hypoxaemia, predictors, re-
to
female ratio of 1.3:1 and105
source-poor.
(26.1) presented with respiratory
Introduction
The burden of hypoxaemia in developing countries is
huge because a large proportion of children are brought
Hypoxaemia has been recognised as a sign of serious ill-
into the hospital in serious condition requiring emer-
gency care. Subhi and his group in a systematic re-
5
6
health in children because it often denotes poor ventila-
tion and or perfusion and an urgent need for oxygen
view estimated that 13% (1.5 - 2.7 million) children
therapy.
1-2
Oxygen supply in busy emergency units of
with pneumonia in developing countries who presented
to
health facilities annually are hypoxaemic. Emordi
et
6
resource constrained developing countries is not always
al also
reported that
13% of
children aged
2 to
59
7
available and or affordable. Sometimes oxygen supply
3
is
rationed among children who need it because de-
months admitted to the children emergency unit of a
mands often outweigh supply.
3-4
Ill children are often
tertiary centre in South East Nigeria were hypoxaemic.
7
not well screened for need for oxygen therapy because
Orimadegun et
al however reported a much higher
8
of
the non-availability of pulse oximeters and similar
prevalence of 28.6% among emergently ill neonates and
facilities. These often lead to denial of oxygen therapy
4
children at another tertiary facility in Nigeria and a
to
children whose survival depends on this life-saving
much higher prevalence of 49.2% among those with
respiratory tract infections. Other studies from develop-
8
therapy.
3-4

274
ing
countries including the west African sub region also
Subject recruitment
reported a huge burden of hypoxaemia among ill chil-
dren.
9-12
Unfortunately oxygen supply to meet this huge
Consecutive admissions into the CEW whose parents/
demand is not always available in most of the centres .
3-
caregivers gave consent were recruited for the study.
4
A
large proportion of emergently ill children in devel-
Children admitted with all forms of shock were ex-
oping countries particularly those with non-respiratory
cluded because their peripheral oxygen saturation
symptoms may however remain unrecognised and thus
(SPO 2 ) could not be measured
with pulse oximetry due
to
systemic hypo perfusion.
15
untreated as most reported studies on hypoxaemia
The (SPO 2 ) of the re-
among ill children were done on those with respiratory
cruited children were recorded using a portable pulse
symptoms at presentation.
6
oximeter (Nellcor N-200, USA) by a study assistant who
did
not take part in the history taking and subsequent
Many
centres in resource – poor countries still adminis-
management
of the patients. The SPO 2 was
taken using
ter
oxygen to emergently ill children without diagnosing
an
appropriately sized paediatric probe attached to the
hypoxaemiaobjectively.
3-4
This is often due to non-
finger or toes for at least 30 seconds till the reading of
availability of pulse oximeters and other facilities to
the oximeter is stabilised. Hypoxaemia which is the out-
make this diagnosis.
3-4
This brings to the fore a need for
come variable was defined in this study as SPO
2 < 90%.
2,
simple, easily measureable parameters that could guide
5
clinicians in resource-poor centres in prompt recognition
The study variables included age of the patients, sex,
of
hypoxaemia in emergently ill children with or without
and parental socioeconomic class derived using rank
respiratory symptoms to improve survival. This study
assessment of the parents’ highest level of educational
therefore sets out to determine the prevalence and pre-
attainment
and
occupation
as
described
by
Oyedeji. Also of interest were the clinical features at
16
dictors of hypoxaemia among emergently ill children at
the Wesley Guild Hospital (WGH), Ilesa, Nigeria.
presentation including axillary temperature taken using a
low reading clinical thermometer. Hypothermia was
recorded as temperature less than 35 C; subnormal as 35
0
–
36.5 C; normal as 36.5 to 37.5 C; fever as 37.5 to
0
0
Patients and Methods
38.5 C, and hyperpyrexia as >38.5 C.
0
0
5,17
Other features
at
presentation considered included convulsion, diar-
This was a prospective cross sectional study of children
rhoea, cyanosis, pallor and prostration. The study par-
aged 1 month to 14 years admitted over an eight month
ticipants were categorised into those with respiratory
period (January to August, 2015) at the Children Emer-
features and those without respiratory features at presen-
gency Ward (CEW) of the WGH, Ilesa, Nigeria. The
tation. The respiratory features looked for in these chil-
WGH is a tertiary annexe of the Obafemi Awolowo Uni-
dren included fast breathing defined using the WHO cut
versity Teaching Hospitals Complex (OAUTHC),
off thus (respiratory rate >50 cycles per minute in chil-
Ile‑ Ife. The hospital is one of the main
referral centers
dren less than 12 months; > 40cpm in children 1-5 years
providing specialized pediatric care for the communities
and > 30cpm in those > 5 years); noisy breathing includ-
of
Osun, Ondo, and Ekiti States of the South‑ West Ni-
ing
grunting, wheezing and stridor, nasal flaring and
chest in-drawing. Tachycardia was defined as pulse
17
geria. The children emergency ward of the hospital oper-
ates a 24‑ h service and admits about
600 children per
rate> 150 beats per minute in children 1-3 years and >
140 beats per minute for children > 3 years. The nutri-
17
annum. The hospital has functional biochemical, micro-
biological and hematological laboratory services as well
tional status of the children was assessed using Well-
come classification.
18
as
well‑ equipped and staffed radiological
services
The
children were investigated
which also operate on a 24 h basis.
appropriately based on the presentation. Diagnoses was
Ilesa, the largest town in Ijesaland is situated on latitude
made
based on the unit standard protocol and these were
7°35’N and longitude 4°51’E and is about 200 km
in
line with the WHO guidelines for the management of
common childhood illnesses.
17
North‑ East of Lagos a major commercial
nerve center
The outcomes of hospi-
of
Nigeria. Ilesa is home to about 620,000 people with
13
talisation were recorded as discharged home, died, dis-
about 25% of the population being children <5 years and
charged against medical advice (DAMA) and referred to
up
to 40% children <15 years. The people in Ilesa
13
another health facility.
called Ijesa are mainly traders, peasant farmers, artisans,
Ethical clearance for this study was obtained from the
and civil servants.
13
Ethics and Research Committee of the Obafemi
Awolowo University Teaching Hospitals Complex
Study size
(OAUTHC), Ile-Ife, Nigeria with protocol number
ERC/2014/08/05. Informed consent and assent (as ap-
The minimum sample size for this study was estimated
propriate) were also obtained from the study partici-
14
using Fisher’s formula.
With reference 49.2% preva-
pants.
lence of hypoxaemia among emergently ill children
from a previous study, a minimum total of 384 study
8
Data analysis
participants was estimated. Adding attrition rate of about
five percent, total of 402 children were recruited for the
Data were analyzed using SPSS for Windows software
study
version 17.0 (SPSS Inc. Chicago 2008). Differences
between the means (SD) or median (IQR) values of con-
275
tinuous variables were determined using Student’s t‑
test
Results
or
Mann – Whitney U‑ test; while the
differences between
proportions of categorical variables were determined
Over
an eight month study period, a total of 424 chil-
using Pearson’s Chi‑ squared or
Fisher’s exact tests. The
dren were admitted to the CEW, 22 children were ex-
level of significance at a 95% confidence interval was
cluded including 19 who presented with shock and 3
set at P <0.05. Associations between the presence or
children whose parents did not consent to participate in
absence of hypoxaemia and the study variables that gave
the
study. A total of 402 children were recruited for the
significant results were further analyzed with binary
study and form the basis of further analysis. 105
logistic regression to determine the independent predic-
(26.1%) of the children had respiratory features at pres-
tors
of hypoxaemia among the children with or without
entation. Eighty three (20.6%) of the children were hy-
respiratory features at presentation. Results were inter-
poxaemic at presentation, this included 40 (38.1%) of
preted with Odds ratios (OR) and 95 percent confidence
the
105 children with respiratory features and 43
interval (CI). Statistical significance was established
(14.5%) of 297 with no respiratory features at presenta-
when
CI does not embrace unity.
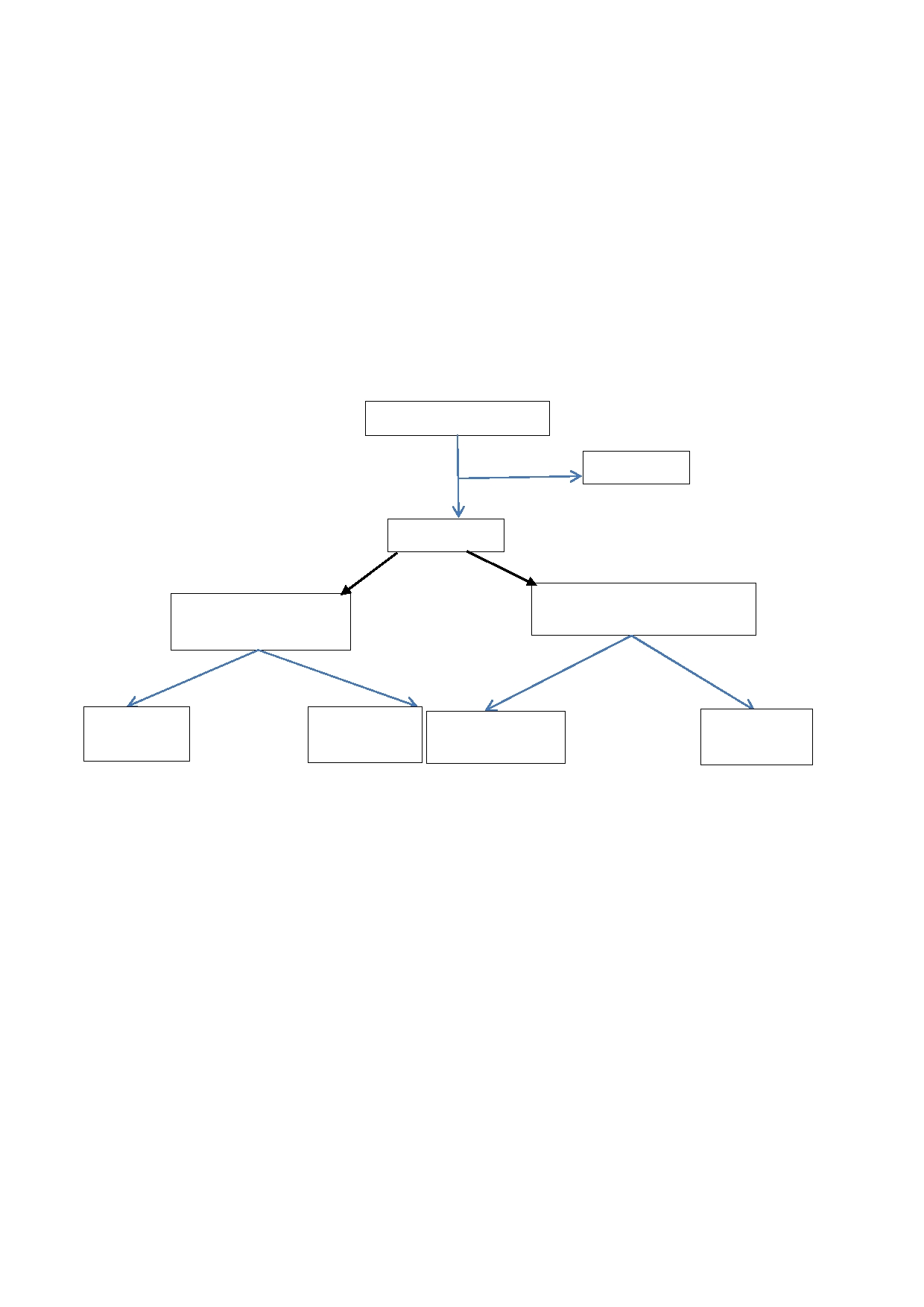
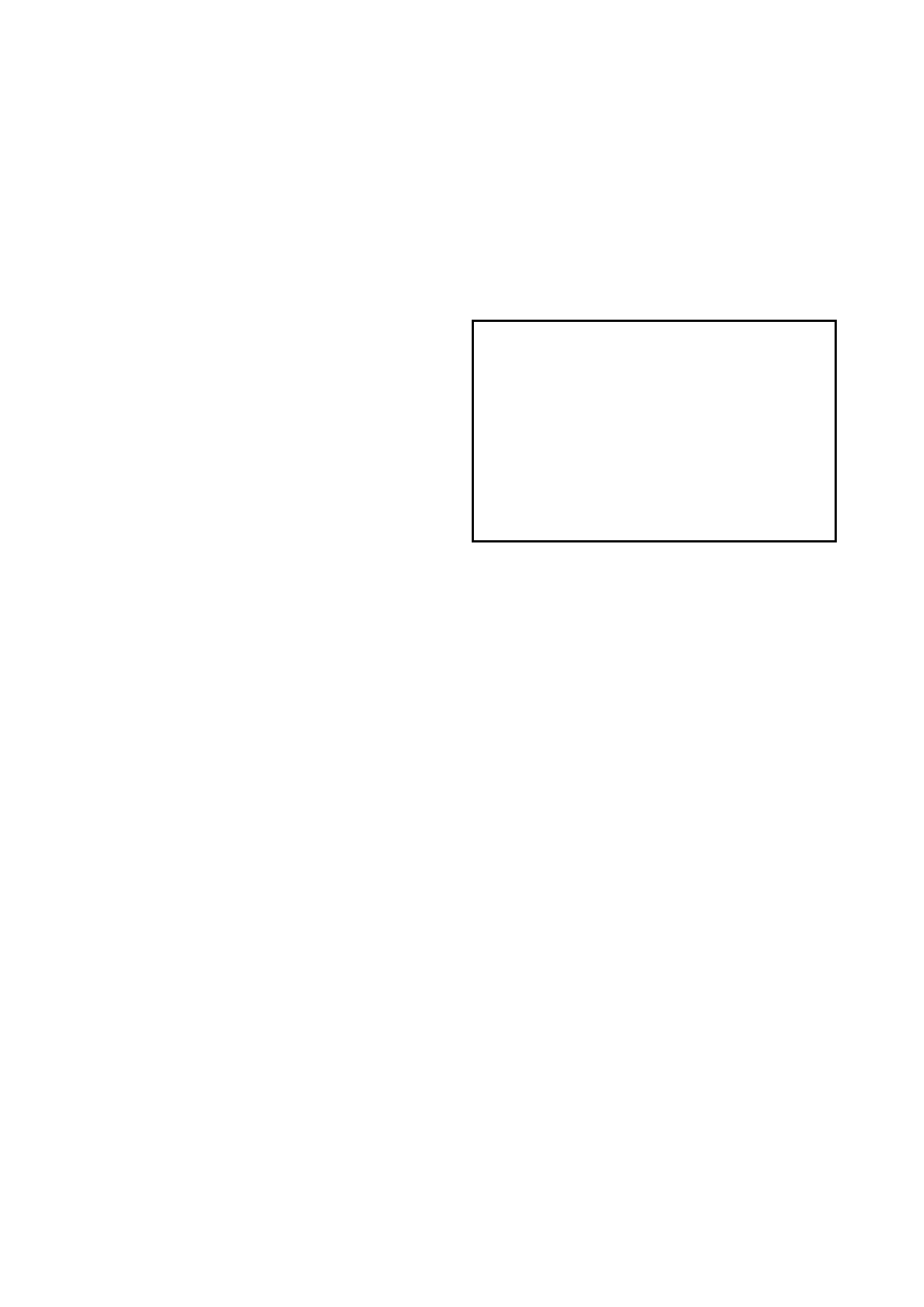
tion. Figure 1 highlights the study participants and
subgroups in a flow chart.
Fig 1: Flow
chart of
the recruitment
of the
study participants
424 children admitted
22
excluded
402 recruited
297 without respiratory features
105 with respiratory
at
presentation
features at presentation
40
were hy-
65
were non-
43
were hypoxae-
254 were non
poxaemic
hypoxaemic
mic
-hypoxaemic
Socio-demographic and general characteristics of the
grunting respiration 12 (11.4); wheezing 10 (9.5%); na-
study participants
sal flaring 50 (47.6%)and chest in-drawing 42 (40.0)
were more commonly observed. Table 2 highlights the
Age and Sex: The
ages of
the children
ranged from
one
clinical presentation of the emergently ill children with
to
168 months with a median interquartile (IQR) age of
or
without respiratory features at presentation. Majority
24
(15 - 42) months. Majority (72.1%) of the children
(82.3%) of the children had normal nutritional status.
were under-fives including 84 (20.8%) infants. Of the
The spectrum of malnutrition observed in the children is
402 study participants, 226 (56.2%) were males with a
also highlighted in table 2.
male to female ratio of 1.3:1.Table one highlights the
The duration of illness before presentation in the 402
socio-demographic characteristics of the study partici-
recruited children ranged from one to 28 days with a
pants as related to the presence or absence of respiratory
median (IQR) of 2 (1-3) days. No significant difference
features at presentation.
in
the Median (IQR) duration of illness before presenta-
Parental socio-economic class:
Majority (77.4%)
of the
tion between the children with respiratory features and
emergently ill children were from middle social class,
those without respiratory features. (Mann Whitney U
while only 31 (7.7%) were from upper social class.
=14973.500; p = 0.716) Majority (74.9%) of the
children presented within three days of illness.
Clinical features at presentation
Fever was the most prominent feature at presentation
reported in 352 (87.6%) of the children. Others present-
ing features included convulsions 152 (37.8%) pallor
138 (34.3%), cough (19.2), vomiting 48 (11.9%) and
loss of consciousness 52 (12.9%).Among the 105 chil-
dren with respiratory features, tachypnoea 90 (85.7%);

276
Table 1: Socio-demographic
and general
characteristics of
the
Factors associated with hypoxaemia among the children
study
participants as related to the presence or absence of res-
piratory symptoms at presentation
Among the children with respiratory features: Infancy
Socio-demographic
Children with
Children with
Total
was significantly associated with the presence of hypox-
features
respiratory
no
respiratory
n =
402
aemia, as 21 (55.3%) of the 38 infants with respiratory
symptoms
features
features compared to 19 (28.4%) of 67 children> one
n =
105 (%)
n=
297 (%)
year were hypoxaemic at presentation (x = 7.443; p <
2
Age range (in years)
0.006). Table III. Conversely, older children (> one
< 1 (infants)
38
(36.1)
46
(15.5)
84
year) were less likely to be hypoxaemic at presentation.
1
-5
55
(52.4)
191
(64.3)
246
The presence of chest in-drawing (52.4% vs. 31.7%;x =
2
6-
14
12
(11.4)
60
(20.2)
72
6.058; p = 0.014), grunting respiration (80.0% vs.
Sex
58.2%; x = 8.148; p = 0.004) and Cyanosis (87.5% vs.
2
Male
63
(63.9)
163
(54.2)
226
57.9%; x = 9.135; p = 0.003) were significantly associ-
2
Female
42
(36.1)
134
(45.8)
176
ated with hypoxaemia among emergently ill children
Parental social class
with respiratory features at presentation. (Table 3)
Upper
class
2
(2.4)
29
(9.1)
31
Among the children with no respiratory features at pres-
Middle class
65
(78.3)
246
(77.1)
311
entation: Infancy was also significantly associated with
Lower class
16
(19.3)
42
(13.2)
58
hypoxaemia among the emergently ill children with no
Place of residence
respiratory features at presentation (x = 5.924; p =
2
Within Ilesa
70
(66.7)
120
(40.4)
190
0.015). Also, pallor (20.6% vs. 14.5%; x = 4.684; p =
2
Outside Ilesa
35
(33.3)
177
(59.6)
212
0.030) and tachycardia (27.3% vs. 14.8%; x = 6.829; p
2
=
0.009) at presentation were significantly associated
The
figures in parentheses are percentages of the total in each
column
with hypoxaemia among the children. (Table 3)
Nutritional status and the presence of hypoxaemia at
Table 2: Clinical
features at
presentation as
related to
the
presence or absence of respiratory features
presentation
Clinical
features at Children with Children with Total
No
significant association was observed between the
presentation
respiratory
no
respira-
n =
402
nutritional status of the children and the presence of
features
tory
features
hypoxaemia at presentation. Table 4 highlights the nu-
n =
105
n =
297
Temp at admission
tritional status of the children with or without respiratory
Hypothermia
1
(1.0)
4
(1.4)
5
features and the presence of hypoxaemia at presentation.
Subnormal
6
(5.7)
11
(3.7)
17
Normal
7
(6.7)
12
(4.0)
19
Outcome of hospitalisation as related to hypoxaemia at
Fever
84
(80.0)
268
(90.2)
352
presentation
Hyperpyrexia
7
(6.7)
2
(0.7)
9
Clinical features
Outcome of hospitalisation:
Majority (93.0%)
of the
DOI median
(IQR)
2.0 (1.0 –
4.0) 3.0 (1.0 – 3.0)
children were discharged home, while 13 (3.2%) of the
Convulsion
20
(19.1)
135
(45.5)
155
children died. (Table 4). The duration of hospitalisation
Pallor
36
(34.3)
102
(34.3)
138
ranged from few hours to 33 days with a median (IQR)
Cough
98
(93.3)
57
(19.2)
77
duration of 3.0 (2.0 – 4.0) days.
Tachycardia
31
(29.5)
44
(14.8)
75
Length of hospitalisation:
Emergently ill
children with
Diarrhoea
4
(3.8)
12
(4.0)
16
hypoxaemia at presentation significantly stayed longer
Coma
2
(1.9)
50
(16.8)
52
in
the hospital compared to non-hypoxaemic children.
Vomiting
10
(9.5)
38
(12.8)
48
(Median (IQR) 4.0 (2.0 – 6.0) days vs. 3.0 (2.0 – 4.0)
Dehydration
5
(4.8)
17
(5.7)
22
days, Mann Whitney U = 9.911, p < 0.001).
Prostration
2
(1.9)
23
(7.7)
25
Mortality: Significantly
more emergently
ill children
Tachypnoea
90
(85.7)
0
(0.0)
100
with hypoxaemia at presentation compared to non-
Nasal
flaring
50
(47.6)
0
(0.0)
50
hypoxaemic children died as 8 (9.6%) of the 83 hypox-
Chest
in-drawing
42
(40.0)
0
(0.0)
42
aemic children compared to 5 (1.5%)of the 329 non-
Stridor
6
(5.7)
0
(0.0)
6
hypoxaemic children, died. The association between
Grunting
12
(11.4)
0
(0.0)
12
Cyanosis
6
(5.7)
2
(0.6)
8
hypoxaemia and mortality is significant irrespective of
Wheezing
10
(9.5)
0
(0.0)
10
the
presence or absence of respiratory symptoms at pres-
Nutritional status
entation as highlighted in table 5.
Normal
80
(76.2)
251
(85.6)
331
Underweight
17
(16.2)
33
(11.9)
50
Predictors of hypoxaemia among emergently ill children
Marasmus
5
(4.8)
10
(2.8)
15
Kwashiorkor
0
(0.0)
1
(0.0)
1
The variables found to be significantly associated with
Overweight/Obese 3 (2.9)
2
(0.9)
5
hypoxaemia among the emergently ill children with or
without respiratory features at presentation (tables 3 and
The figures
in parentheses are percentages of the total in
4)
were further subjected to binary logistic regression
each column.
Temp = temperature; DOI = Duration of ill-
ness before
presentation; IQR = interquartile range
analysis to determine the independent predictors of
277
hypoxaemia. Grunting respiration (OR = 7.875; 95%CI
ergently ill children with respiratory features at the
=
1.029 – 15.797; p = 0.045) and Cyanosis at presenta-
WGH,
Ilesa. However, among the children with no res-
tion
(OR = 13.576; 95%CI 1.360 – 14.279; p = 0.009)
piratory features, none of the variables independently
were independent predictors of hypoxaemia among em-
predict hypoxaemia (Table 6)
Table 3: Socio-demographic
characteristics and
clinical features
of the
children as
related to
the presence
of hypoxaemia
at
presentation
Variables
Children with respiratory features n =
p-value
Children with no respiratory
p
-value
105
features n = 297
Hypoxaemic
Non-hypoxaemic
Hypoxaemic
Non-hypoxaemic
n =
40 (%)
n =
65 (%)
n =
43 (%)
n =
254 (%)
Sex
Male
26
(65.0)
37
(56.9)
0.412
27
(62.8)
136
(53.5)
0.260
Female
14
(35.0)
28
(43.1)
16
(37.2)
118
(46.5)
Age range (years)
< 1
21
(52.5)
17
(26.2)
0.006
12
(27.9)
34
(13.4)
0.015
1 -
5
15
(37.5)
40
(61.5)
<0.001
24
(55.8)
167
(65.7)
0.209
6-
14
4
(10.0)
8
(12.3)
0.716*
7
(16.3)
53
(20.9)
0.479
Social class
Upper
class
1
(2.5)
6
(9.2)
0.151*
1
(2.3)
23
(9.1)
0.087*
Middle class
32
(80.0)
53
(81.5)
0.845
33
(76.7)
195
(76.8)
0.997
Lower class
7
(17.5)
6
(9.2)
0.212
9
(20.9)
36
(14.2)
0.253
Place of residence
Within Ilesa
24
(60.0)
31
(47.7)
0.219
21
(48.8)
133
(52.4)
0.669
Outside Ilesa
16
(40.0)
34
(52.3)
22
(51.2)
121
(47.6)
Clinical features
Temperature
Hypothermia
0
(0.0)
1
(1.5)
0.326*
1
(2.3)
3
(1.2)
0.578*
Subnormal
2
(5.0)
4
(6.2)
0.803*
1
(2.3)
10
(3.9)
0.583*
Normal
2
(5.0)
5
(7.7)
0.584*
3
(7.0)
9
(3.5)
0.327*
Fever
33
(75.0)
51
(86.2)
0.615
38
(88.4)
230
(90.6)
0.656
Hyperpyrexia
3
(7.5)
4
(4.6)
0.790*
0
(0.0)
2
(0.8)
0.428
Other features
Convulsion
4
(10.0)
16
(24.6)
0.064*
14
(32.6)
111
(45.7)
0.171
Pallor
12
(30.0)
24
(36.9)
0.468
21
(48.8)
81
(31.8)
0.030
Tachycardia
13
(32.5)
18
(27.7)
0.600
12
(27.9)
32
(12.6)
0.009
Diarrhoea
3
(7.5)
10
(15.4)
0.219*
4
(1.6)
14
(5.5)
0.363*
Coma
2
(5.0)
3
(4.6)
0.929*
2
(4.7)
13
(5.1)
0.896*
Vomiting
5
(12.5)
12
(18.5)
0.242
8
(18.6)
57
(22.4)
0.574
Dehydration
3
(7.5)
2
(3.1)
0.412*
3
(7.0)
14
(5.5)
0.710*
Prostration
1
(2.5)
1
(1.5)
0.730*
1
(2.3)
22
(8.7)
0.102*
Nasal flaring
20
(50.0)
30
(46.2)
0.702
0
(0.0)
0
(0.0)
NA
Chest in-
22
(55.0)
20
(30.7)
0.014
0
(0.0)
0
(0.0)
NA
drawing
Tachypnoea
32
(80.0)
58
(89.2)
0.189
0
(0.0)
0
(0.0)
NA
Stridor
2
(5.0)
4
(6.2)
0.803*
0
(0.0)
0
(0.0)
NA
Grunting
8
(20.0)
2
(3.1)
0.004*
0
(0.0)
0
(0.0)
NA
Wheezing
4
(10.0)
4
(6.2)
0.477*
0
(0.0)
0
(0.0)
NA
Cyanosis
7
(17.5)
1
(1.5)
0.003*
0
(0.0)
0
(0.0)
NA
The
figures in parentheses are percentages of the total in each column.* Fisher’s
exact test applied. NA = not applicable
Table 4: Nutritional
status of
the study
participants in
relation to
the presence
of hypoxaemia
at presentation
Variables
Children with respiratory features n
p-value
Children with no respiratory features n
p
-value
=
105
=297
Hypoxaemic
Non-hypoxaemic
Hypoxaemic n =
Non-hypoxaemic n
n =
40 (%)
n =
65 (%)
43
(%)
=
254 (%)
Normal
32
(80.0)
48
(73.8)
0.472
36
(83.7)
219
(86.2)
0.664
Underweight
5
(12.5)
12
(18.5)
0.421
4
(9.3)
29
(11.4)
0.737
Marasmus
2
(5.0)
3
(4.6)
0.929
1
(2.3)
5
(2.0)
0.891
Kwashiorkor
0
(0.0)
0
(0.0)
NA
1
(2.3)
0
(0.0)
0.401
Overweight/Obese
1
(2.5)
2
(3.1)
0.663
1
(2.3)
1
(0.4)
0.245
The
figures in parentheses are percentages of the total in each column.* Fisher’s
exact test applied
278
Table 5: Outcome
of hospitalisation
as related
to the
presence of
hypoxaemia at
presentation
Outcome
Children with respiratory features n = 105
p-value
Children with no respiratory features n = 297
p
-value
Hypoxaemic n =
Non-hypoxaemic
Hypoxaemic n = 43
Non-hypoxaemic n =
40
(%)
n =
65 (%)
(%)
254
(%)
Discharged
36
(90.0)
61
(93.8)
0.473
38
(88.4)
239
(94.1)
0.101
DAMA
0
(0.0)
2
(3.1)
0.163*
1
(2.3)
10
(3.9)
0.583*
Died
4
(10.0)
1
(1.5)
0.049*
4
(9.3)
2
(1.2)
0.003*
Referred
0
(0.0)
0
(0.0)
NA
0
(0.0)
1
(0.4)
0.576*
The
figures in parentheses are percentages of the total in each column; DAMA =
discharged against medical advice. * Fisher’s
exact test applied
Table 6: Predictors
of hypoxaemia
among emergently
ill children
with or
without respiratory
features at
presentation using
multiple regression analysis
Variables
Coefficient of
Standard
Odds ratio
95%
confident interval
P value
regression
error
Respiratory features
Infancy
0.801
0.495
3.121
0.845 - 5.871
0.105
Grunting respiration
1.394
0.697
7.875
1.029 - 15.797
0.045
Cyanosis
1.211
0.461
13.576
1.360 - 14.279
0.009
Chest in-drawing
0.955
0.476
2.750
0.768 - 4.778
0.098
No respiratory features
Infancy
0.741
0.613
2.179
0.631 - 6.971
0.227
Pallor
1.059
0.560
2.360
0.146 - 7.167
0.054
Tachycardia
0.136
0.610
2.973
0.347 - 3.787
0.824
Diagnostic accuracy of predictors
: Grunting
respira-
inspiring against a partially closed glottis. It is a form of
2
tion among children with respiratory features has a sen-
positive pressure ventilation employed by ill children to
sitivity of 20.0%; specificity of 96.9%; positive and
overcome ventilation perfusion mismatch caused by
negative predictive values of 44.4% and 66.3% respec-
conditions that can result in increased lung dead space.
2
tively. Cyanosis among children with respiratory fea-
Inability of the compensatory mechanisms like grunting
tures has a sensitivity of 17.5%, specificity of 98.5%,
and use of accessory respiratory muscles to improve
positive and negative predictive values of 87.5% and
oxygenation often results in the build-up of deoxygen-
ated haemoglobin in the circulation. This often mani-
2
66.0% respectively.
fests clinically as cyanosis hence grunting respiration
and cyanosis are important predictors of hypoxaemia in
sick children with high specificity. However the absence
Discussion
of
grunting and cyanosis in sick children does not
exclude hypoxaemia as their sensitivity to detect hypox-
This
study has highlighted the prevalence and simple
aemia is low as observed in this study.
measurable predictors of hypoxaemia among ill children
at
the emergency unit of a resource poor centre. The
Sick Infants were observed in this study to be at in-
20.6% prevalence of hypoxaemia reported in this study
creased risk of having hypoxaemia compared to older
is
similar to reported prevalence of 19.0% in the Gambia
children. These findings were corroborated by studies
9-12
within and outside Nigeria.
8
by
Junge et
al using the same criteria. This is however,
19
This may be due to the
much higher than 13.3% reported by Emodi
et al from a
7
fact that infants have low tidal volume and relative inef-
tertiary centre in Nigeria. This difference between the
ficient compensatory mechanisms (like use of accessory
prevalence of hypoxaemia in this study compared to that
respiration muscles) to improve ventilation. In situations
of
Emodi et
al may be explaint by relative smaller sam-
7
of
increased dead space and ventilation perfusion mis-
ple size (92 children) studied by the latter compared to
match, infants are poorly equipped to compensate for
this, thus they easily succumb to hypoxaemia. Conse-
2-3
402 children recruited in this study. The prevalence of
20.6% observed in this study is much less than 52.0%
quently, ill infants should particularly be carefully as-
reported by Dukes et
al in Papua New Guinea. The
1 9
sessed for hypoxaemia at presentation and promptly
higher prevalence reported from Papua New Guinea
treated to ensure survival.
may be due to fact that it is located in a high altitude
region (1600m above sea level) with expected relative
In
addition to infancy, pallorand tachycardia were also
ambient hypoxia compared to the present study which
observed to be associated with hypoxaemia among the
was conducted at sea level.
children with no respiratory features at presentation.
This observation was corroborated by Emordi
et al who
7
Cyanosis and grunting respiration were observed to pre-
reported higher frequency of anaemia among hypoxae-
dict hypoxaemia among children with respiratory fea-
mic children in Enugu, Nigeria. Severe anaemia is the
tures in this study. This is similar to reported observa-
most common cause of pallor among emergently ill chil-
dren in malaria endemic region like our study site. Se-
5
tions in other studies in developing countries among
children with pneumonia and respiratory tract infec-
verely anaemic children may often be hypoxaemic due
tions
9-12
Grunting is an inspiratory sound produced by
to
inability of the depleted haemoglobin to carry enough
279
oxygen to meet the tissue requirements. (Anaemic hy-
ratory features at presentation and one in every seven
poxia)
2
Anaemic heart failure can also ensue in these
children with no respiratory features at presentation in
children leading to pulmonary congestion and poor ven-
Ilesa, Nigeria. The presence of hypoxaemia was signifi-
tilation and perfusion. This explains why tachycardia
2
cantly associated with mortality irrespective of the pre-
and pallor were significantly associated with the pres-
senting features. Emergently ill children in resource-
ence of hypoxaemia among the emergently ill children.
poor settings who presented with respiratory features
Hypoxaemia was observed in this study to be associated
and cyanosis, grunting respiration and chest in-drawing
with mortality irrespective of the presenting features.
and those with no respiratory features but presented with
This finding was also reported by other researchers in
pallor and tachycardia especially infants should prefer-
children with or without respiratory symptoms.
7-12, 19-20
entially be placed on oxygen therapy even when hypox-
Hypoxaemia often connote poor tissue oxygenation with
aemia had not been confirmed.
consequent impair aerobic respiration and cellular en-
ergy utilisation. This impaired cellular functions includ-
2
ing sodium/potassium ATP pump ultimately leading to
Author’s contributions
cellular damage and death. This implies that hypoxae-
2
Kuti BP: Conceptualised the study, collected, analysed
mia should be promptly recognised and managed effi-
the data and wrote the manuscript
ciently particular in sick children to improve survival.
Adetola HH: Collected the data and revised the
We
appreciate the limitation that oxygen saturation
manuscript
(SPO 2 ) was assessed once at
presentation in the study
Kuti DK: Participated in data collection and analysis.
participants and preferred continuous oxygen monitor-
Also revised the manuscript
ing in sick children was not done due to unavailability of
Aladekomo TA: Supervised the conduct of the study and
facilities to do so. Nonetheless, this study has high-
revised the manuscript.
lighted simple easily observable factors that can guide
All the authors approved the final manuscript.
clinicians in resource poor in prompt detection of hy-
Conflicts of interest :
None
poxaemia among emergently ill children with or without
Funding :
None
respiratory features at presentation even in the absence
of
facilities to detect and monitor hypoxaemia.
Acknowledgements
Conclusion
The authors acknowledge the contributions of the clini-
cians and nurses at the children emergency wards of the
In
conclusion, at the emergency room, hypoxaemia was
WGH, Ilesa who participated in the care of the children.
present in one of every two to three children with respi-
References
1.
Duke T, Graham SM, Cherian
5.
Management of the child with a
8.
Orimadegun AE, Ogunbosi
MN, Ginsburg AS, English M,
serious infection or severe mal-
BO, Carson SS.Laman M,
Howie S, et al. The Union
nutrition. World Health Organi-
Ripa P, Vince J, Tefuarani N.
Oxygen Systems Working
zation, Geneva, 2000.
Prevalence and predictors of
Group. Oxygen is an essential
6.
Subhi R, Adamson M, Camp-
hypoxaemia in respiratory and
medicine: a call for interna-
bell H, Weber M, Smith K,
non-respiratory primary diag-
tional action Int
J Tuberc
Lung
Duke T, for the Hypoxaemia in
noses among emergently ill
Dis . 2010; 14(11): 1362 – 8.
Developing Countries Study
children at a tertiary hospital
2.
Qureshi SA. Measurement of
Group. The prevalence of hy-
in
south western Nigeria.
respiratory function: an update
poxaemia among ill children in
Trans R Soc Trop Med Hyg .
on
gas exchange. Anaesthesia
developingcountries: a system-
2013; 107:699-705.
& Intensive Care Medicine
atic review. The
Lancet 2009;
9.
Basnet S, Adhikari R, Gurung
2011; 12: 490 – 5.
9: 221-227.
C.
Hypoxemia in children
3.
Wandi F, Peel D, Duke T. Hy-
7.
Emodi J, Ikefuna AN, Ubesie
with pneumonia and its clini-
poxaemia among children in
AC, Chukwu BF, Chinawa JM.
cal predictors. Indian
J Pedi-
rural hospitals in Papua New
Assessment of clinical features
atr. 2006; 73:777 – 81.
Guinea: epidemiology and re-
andhaematocrit levels in detec-
10. Laman
M, Ripa
P, Vince
J,
source availability — a study to
tion ofhypoxaemia in sick chil-
Tefuarani N. Can clinical
support a national oxygen pro-
dren. AJRM
2011; 7(1):
11-13.
signs predict hypoxaemia in
gram. Ann
Trop Paediatr
2006;
Papua New Guinean children
26:277 – 284.
with moderate and severe
4.
Schneider G. Oxygen supply in
pneumonia? Ann
Trop Pedi-
rural Africa: a personal experi-
atr . 2005; 25: 23 – 7.
ence. Int
J Tuberc
Lung Dis
2003; 5: 524 – 6.

280
11. Usen S, Webert M. Clinical
15. Bohnhorst B, Peter CS, Poets
19. Junge S, Palmer A, Green-
signs of hypoxaemia in chil-
CF. Pulse oximeters’ reliability
word BM, Mulholland EK,
dren with acute lower respira-
in
detecting hypoxaemia and
Weber MW. The spectrum of
tory infection: indicators of
bradycardia: comparison be-
hypoxemia in children admit-
oxygen therapy. Int
J Tuberc
tween a conventional and two
ted to hospital in Gambia,
Lung Dis . 2001; 5: 505 – 10.
new generation oximeters. Crit
West Africa. Trop
Med Int
12. Kuti BP, Adegoke SA, Ebruke
Care Med 2000; 28:1565-8.
Health 2006; 11: 367 – 72.
BE, Howie S, Oyelami OA,
16. Oyedeji GA. Socioeconomic
20. Duke T, Blaschke AJ, Sialis
Ota M. Determinants of Oxy-
and cultural background of
S,
Bonkowsky JL. Hypoxae-
gen Therapy in Childhood
hospitalized children in Ilesa.
mia in acute respiratory and
Pneumonia in a Resource-
Niger J Paediatr 1985;
non-respiratory illnesses in
Constrained Region. ISRN
Pe-
13:111‑
8.
neonates and children in a
diatrics. 2013;
Article ID
17. WHO. Pocket book of hospital
developing country. Arch
Dis
435976, 6 pages
care for children: guidelines for
Child 2002; 86:108-112.
13. Ilesa West Local Government
the management of common
Area. Available from: http://
illnesses with limited resources.
www.info@ilesawestlg.os.gov.
World Health Organization,
ng. [Last accessed 23 Septem-
rd
Geneva; 2005
ber, 2015].
18. Well come Trust Working
14. Araoye MO. Subjects Selec-
Party. Classification of infantile
tion. In: Araoye MO, editor.
malnutrition. Lancet
1970;
Research methodology with
2:302- 3.
statistics for health and social
sciences. 1 ed. Ilorin: Natadex
st
2003:115-21.







