

Copyright 2015 © Nigerian Journal of Paediatrics. All Rights Reserved. . Powered by Pelrox Technologies Ltd
ISSN 03 02 4660 AN OFFICIAL JOURNAL OF THE PAEDIATRIC ASSOCIATION OF NIGERIA


Quick Navigation

Niger J Paediatr 2016; 43 (4): 295 – 298
CASE
REPORT
Eke GK
Hereditary multiple exostoses in a
Omunakwe HE
Echem RC
15-year-old boy: A case report
and review of literature
DOI:http://dx.doi.org/10.4314/njp.v43i4.12
Accepted: 6th September 2016
Abstract :
Background: Heredi-
These swellings were non-tender,
tary Multiple Exostoses (HME) is
not attached to the overlying skin
Eke
GK (
)
a
rare bone disease, usually asso-
and immobile, had no differential
Department of Paediatrics,
ciated with deformity and pres-
warmth and appeared to be con-
Omunakwe HE
sure symptoms. It is an autosomal
tinuous with the underlying bony
Department of Haematology
dominant disorder characterized
structures. A striking feature was
by
the development of benign
exostoses that extended from the
Echem RC
tumours growing outward from
lumbar spine towards the left scap-
Department of Orthopaedics,
the
metaphyses of long bones and
ula.
He also had brachymetatarsia
University of Port Harcourt Teaching
can
lead to considerable psycho-
of
the first ray of both feet. Skele-
Hospital, Port Harcourt, Rivers State,
social problems. This paper aims
tal
survey confirmed the diagnosis.
Nigeria.
at
reporting a case of HME with
Conclusion: Though
rare, HME
do
Email: kergracia@yahoo.com
some peculiar features.
occur in our environment. The
Methods: A
case report
of a
15-
treatment is individualized, with
year-old Nigerian male with He-
small asymptomatic or minimally
reditary Multiple Exostoses is
symptomatic lesions followed up
presented to highlight the clinical,
and only supportive care provided.
radiological features and manage-
Larger symptomatic lesions may
ment challenges of the condition.
cause major physical handicap and
Results: The
patient presented
may be resected.
with multiple hard, bony and
ridge-like growth along the spine,
Key words :
Hereditary, Multiple,
scapula and para-vertebral region
Exostoses, Deformity
which gradually increased in size.
Introduction
It
manifests more in early childhood to puberty and
40% of the affected children manifest before the age of
Osteochondroma, the most common bone tumour seen
10
years. Lesions have been infrequently reported to
in
children, is a developmental lesion rather than a true
spontaneously regress during the course of childhood
and puberty.
3,10
neoplasm and constitutes 20% – 50% of all benign bone
tumours. It is a cartilage-capped exostosis found pri-
1
The commonest complications of this condition are de-
marily at the juxta-epiphyseal region of the most rapidly
formity, pressure symptoms and malignant degenera-
growing ends of long bones.
2
Hereditary Multiple
tion.
1,3,4,5
Diagnosis is based on clinical examination and
Exostosis (HME), also known as diaphyseal aclasia and
radiographic evaluation, while treatment of osteochon-
multiple osteochondromatosis, is characterized by the
droma is individualized, depending on the presentation.
In
Nigeria, cases of HME have also been reported,
11,12
development of multiple osteochondromas (exostoses)
and is frequently associated with characteristic progres-
affecting the lower and upper limbs while the index pa-
sive skeletal deformities.
3-6
The
disorder shows an auto-
tient had in addition massive exostoses which extended
somal dominant inheritance pattern with approximately
from the lumbar spine towards the left scapula. This was
two-thirds of affected individuals having a positive fam-
not a common feature in cases reported in the literature.
ily history. The earliest known description of an af-
1
The aim of this paper is to report a case of hereditary
flicted family was reported by Boyer in 1814.
3,7
multiple exostoses with some peculiar features.
The true prevalence of HME is not known since many
patients with asymptomatic lesions are never diag-
Case report
nosed. However, its estimated prevalence is 1:50,000 to
3
1:100,000 in Western populations and may be as high as
K.V, a 15-year old Nigerian male was referred from a
1:1,000 in the Chamorros, the indigenous people of
public secondary level health care facility and presented
Guam and the Mariana Islands.
1,8
Although previously
to
the Children Out-patient Clinic of the University of
thought to have a male predominance, HME now ap-
Port Harcourt Teaching Hospital (UPTH) in Rivers
pears to affect both sexes similarly.
3,9
State, Nigeria because of a 3-year history of multiple
296
swellings on the back.
These developed over his lower back along the midline
and
over the lateral and upper aspects of his back as
multiple swellings which gradually increased in size and
eventually coalesced in certain areas, causing a deforma-
tion of his back with difficulty in bending his trunk and
inability to freely turn his head to both sides. He had
mild pain when lying on his back. There was no preced-
ing history of trauma and no other constitutional symp-
toms.
He
had herbal concoctions with scarifications before
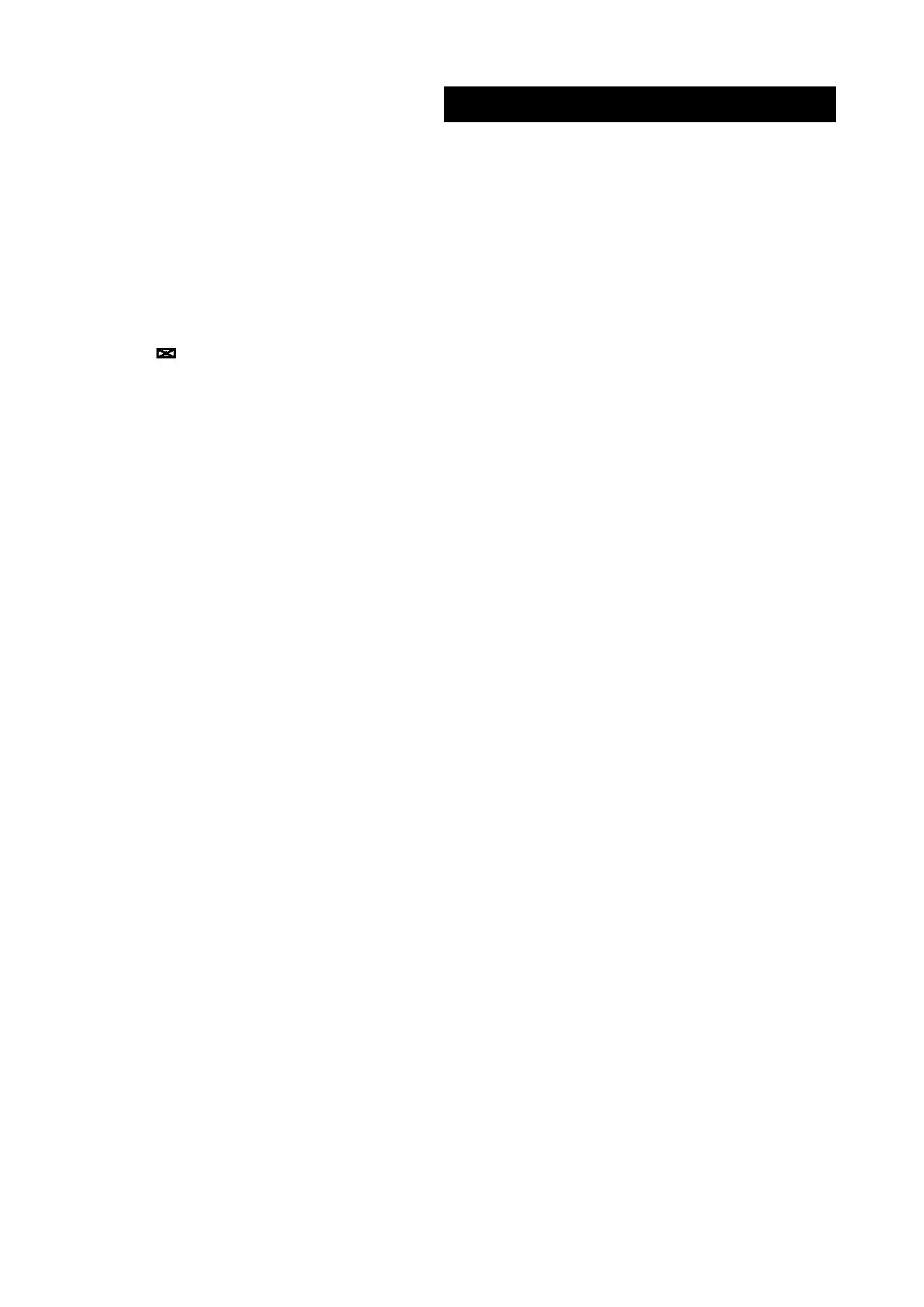
Fig 1a: Photograph
of the
Fig 1b: Photograph
of a
closer
presenting at the referral health facility for worsening of
patient’s back
view of the legs and feet
limitation of movements of the neck and trunk.
He
was said to have developed similar swellings at 10
months of age over his trunk, no x-ray was done for con-
firmation,which lasted about 6 months and regressed
spontaneously. However they re-occurred 3 years prior
to
presentation, when patient was 12 years old.
An
average grade 7 student (JSS1), he had not attended
school for the last 1 year because of worsening limita-
tion of his movements. He is the last of 8 children, 5
alive, in a monogamous family setting. His mother was
a
farmer with no formal education, while his father died
of
a chronic illness 7 years prior to child's presentation.
There was no history of similar illness in the family and
they reside in an oil producing area of the Niger Delta
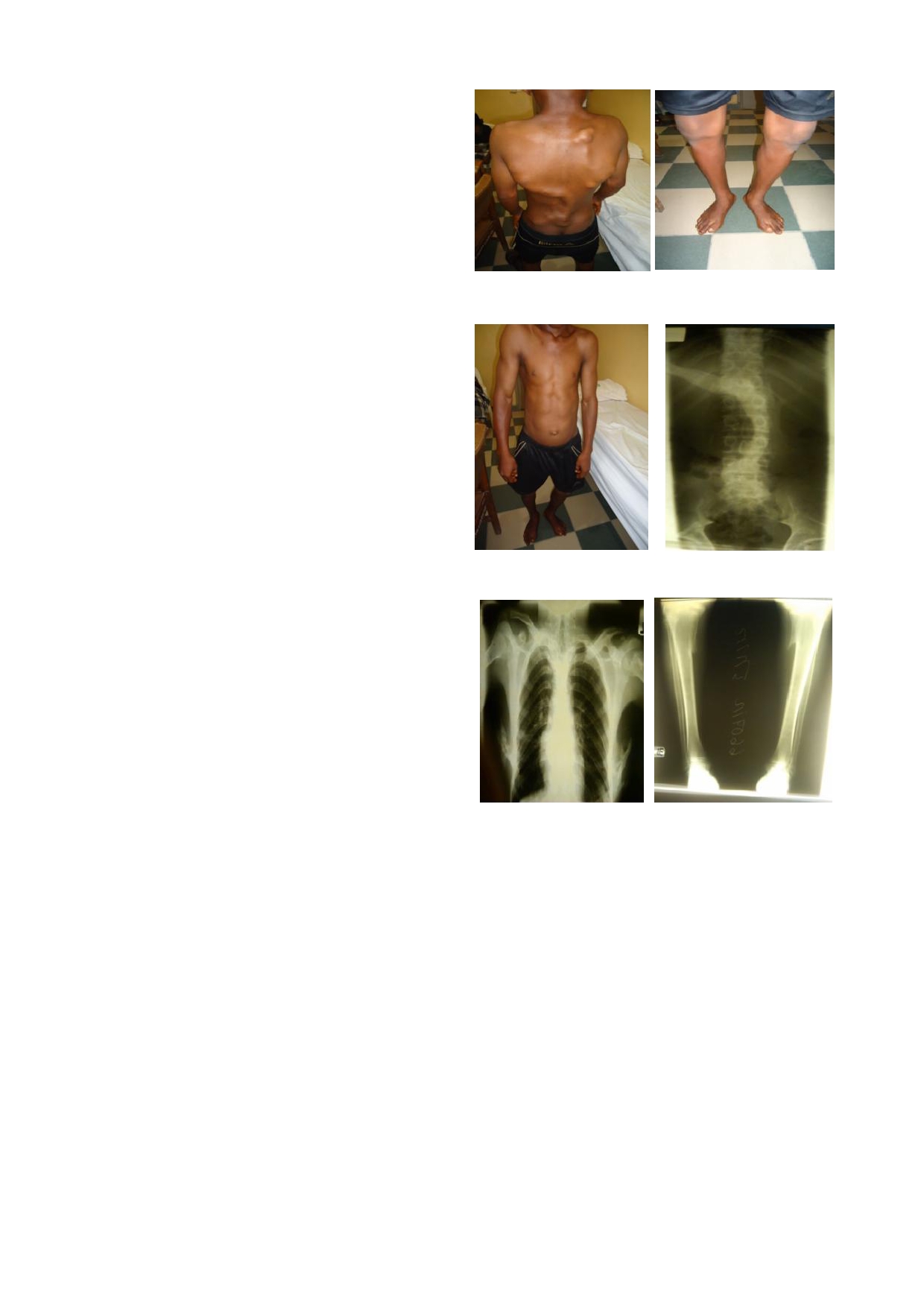
Fig 1c: Photograph
of the
patient Fig 2: X-ray of
thoraco-
region with petroleum exploratory activities and recur-
lumbar spine from the front
rent oil spillages in the community as well as past his-
tory of communal clashes with use of explosives and
other local war artillery. Their source of drinking water
is
well water which is not boiled.
Physical examination revealed a withdrawn adolescent,
in
no obvious respiratory or painful distress. There was
asymmetry of the pectoral girdle, marked left-sided sco-
liosis, neck stiffness with limited rotational movement
of
the head. Masses along the spine, scapula and para-
vertebral regions were multiple, hard, bony, rounded and
ridge-like, some measuring up to 6x8cm, non-tender, not
attached to the overlying skin and immobile, with no
Fig 3: Chest
X-ray showing
Fig 4: X-ray
of both
legs
differential warmth, appearing to be continuous with the
exostoses from rib cage
showing exostoses at the
underlying bony structures (Fig1). There were also knob
proximal tibia
-like hard bony swellings over the lateral aspect of the
upper one-third of the left leg with a similar protrusion
over the right lateral maleoli. He had brachymetatarsia
of
the first ray of both feet (Fig1). There was no neuro-
Discussion
logical deficit. His height was 156cm. Skeletal survey
(Fig.2,3 and 4) confirmed the diagnosis of HME.
Hereditary Multiple Exostoses (HME) is a genetically
He
was admitted for investigations and co-managed
heterogeneous disorder and has been associated with
with
the orthopedic surgeons, physiotherapist and social
mutations in at least three different genes, termed EXT
workers. Counselling was offered, excision of some of
genes. At least two of these genes are thought to func-
tion as tumour suppressor genes.
3,4,6
the
exostoses especially those on the back was advised
These mutations
as
well as genetic studies.However, he signed against
may disrupt normal cartilage growth, resulting in the
formation of an osteochondroma. The three described
3
medical advice, stating financial constraints as main
reason, and had since been lost to follow up.
EXT loci have been recently mapped: EXT1 on chromo-
some 8q23-q24, EXT2 on 11p11-p12, and EXT3 on
chromosome 19p. According to linkage analysis, the
EXT1 and EXT2 loci appear to be altered in the major-
ity of families while, EXT3, which has not been fully
isolated and characterized, is probably less frequently
affected.
3,4,6
Epidemiologic analysis of linkage and mu-

297
tation data indicate that mutations of EXT1 and EXT2
the
late presentation. Osteochondromas that extend ante-
are
likely to be responsible respectively for one half and
riorly from the vertebral body may produce symptoms
one
third of MHE cases. Genetic studies were however
of
dysphagia, hoarseness, and vascular compromise.
not
conducted for the index patient.
Affected individuals may also show disturbance of
growth with short stature, wrist and ankle deformity and
Hereditary Multiple Exostoses is characterized by for-
mental handicap as had been reported by other workers
9,17
mation of ectopic, cartilage-capped, growth plate-like
but these features are variable and were not seen in
exostoses next to growing long bones and other skeletal
the index case.
elements. The exostoses usually originate proximal to
an
active growth plate, may occur at or after birth and
The index patient had a history of similar swellings
throughout puberty, and may continue to grow slowly
around the trunk at the age of 10 months, which re-
3,9,13
during adulthood.
They form predominantly on the
gressed spontaneously after about 6 months. Earliest
physes of long bones, pelvis, ribs, scapula, and vertebrae
lesions may even be present at birth as had been re-
ported by Solomon. On the other hand, though uncom-
9
and
begin to appear as early as 2 years of age.
9,11,14
Most
patients are diagnosed by age 5 years, and virtually all
mon phenomena, the pattern of spontaneous resolution,
are diagnosed by age 12 years. In families with the ge-
or
appearance of new lesions years after excision of pri-
netic predisposition, members who do not demonstrate
mary osteochondromas have been previously docu-
mented, but the literature is limited.
10,18
lesions by age 12 years will not manifest the disease.
Brachymetatarsia
After adolescence and skeletal maturity, osteochondro-
of
the first ray of both feet were present in the index
mas usually exhibit no further growth.
1
patient. The feet can be involved in HME as had been
reported by other workers.
8,9
There is scarcity of reported cases of MHE in Nigeria.
This may be because of under-reporting rather than non
Complications commonly associated with these exo-
occurrence seeing that two reports of this rare autosomal
phytic masses include cosmetic and osseous deformity,
dominant disorder were found. Yinusa
et al reported 2
pressure symptoms, fracture, vascular compromise, neu-
cases, a 13-year-old girl and a 9-year-old boy, who pre-
rologic sequelae, overlying bursa formation, and malig-
sented at an orthopaedic hospital within a six months
nant transformation. Of these, outstanding complications
period, whilst Adelowo and Adebayo reported the dis-
11
in
the index patient were cosmetic deformity, restricted
ease in two siblings, both of whom are children of an
joint movements affecting the vertebral joints, the upper
achondroplastic father.
12
and lower limbs and pain. This is of great concern as the
patient was already out of school because of these com-
Whereas all cases reported in Nigeria presented with
plications, possibly facing physical, psychological and
clinical and radiological features of HME affecting the
social distress which have a negative impact on his qual-
lower and upper limbs, the index case had in addition
ity of life.
massive exostoses on the spine, scapulae and ribs (Fig.1,
Fig 2, Fig 3 and Fig 4). One of the peculiar features with
Malignant transformation has been reported, with docu-
this patient was the exostoses which extended from the
mented risk of 1-6% in patients with HME in adulthood,
lumbar spine towards the left scapula, an unusual feature
with chondrosarcoma developing more frequently than
osteosarcoma.
1,3-5,8,9,17,19
in
cases reported in the literature. We wonder if there
Higher estimates of 10-25%
could be any factors responsible for the elongation. This
have been cited but they have been a function of bias
is
a subject that will require further research.
and incomplete detection of affected individuals who did
not have a sarcoma but were members of a family that
had exostoses.
8,9
Central exostoses involving the skull base, spine, or rib
Lesions that grow or cause pain after
heads are seen in 1% – 9% of patients with HME, and
skeletal maturity should be suspected of malignant
may cause cranial nerve deficits, radiculopathy, spinal
transformation which is distinctly unusual before the age
stenosis, cauda equina syndrome, myelomalacia and
of
20. The index patient should therefore be kept under
spinal cord compression.
1,15,16
Interestingly, in patients
regular review both clinically and radiologically to
with HME, spinal lesions are usually solitary. The cervi-
evaluate progression of deformities and development of
cal spine is most frequently affected (50% of lesions),
complications.
followed by the thoracic and the lumbar spine. Lesions
The diagnosis depends largely upon X-rays while the
that protrude dorsally from the posterior vertebral ele-
radiographic appearance of a lesion composed of bone
ments (lamina or spinous process) are typically large
demonstrating cortical and medullary continuity with the
underlying parent bone is often pathognomonic. Le-
1
and manifest at an earlier age with cosmetic deformity
and palpable mass but lack neurologic symptoms. In
sions that involve complex areas of anatomy (spine or
contradistinction, osteochondromas that extend into the
pelvis) are frequently better assessed with CT or MR
spinal canal are often small but are associated with neu-
imaging to detect the characteristic marrow and cortical
continuity.
16,20
rologic symptoms. It is therefore not surprising that
1
Bone
scintigraphy has been demonstrated
despite the considerable size of the spinal lesions caus-
to
be useful in the periodic surveillance of adult patients
with
HME.
21
ing limitation of range of flexion and extension of the
A
biopsy should be done in doubtful cases
and
to help assessing malignant degeneration.
19
trunk and significant deformity, the index patient had no
neurological deficit. The fact that the deformity was on
Differential diagnosis include Dysplasia Epiphysealis
the back, usually covered with cloths, could account for
Hemimelica (DEH) or Trevor's disease, which is

298
transmitting the disorder to his offspring.
4,7,22
described as a type of over growth at one or more
epiphyses, and metachondromatosis, a rare disorder that
exhibit symptoms of both multiple osteochondromas and
enchondromas in children and is also inherited in auto-
somal dominant mode.
4
Conclusion
Treatment of HME is individualized and much more
problematic and complex than that of patients with soli-
Though rare, HME do occur in our environment. The
tary osteochondromas. Small asymptomatic or mini-
treatment is individualized, with small asymptomatic or
mally symptomatic lesions are followed up and only
minimally symptomatic lesions followed up and only
supportive care provided while larger symptomatic le-
supportive care provided. Larger symptomatic lesions
sions may be resected. Thus, depending on the deform-
may cause major physical handicap and may be
ity, the surgical intervention may involve corrective os-
resected.
teotomy, epiphysiodesis, excision or limb lengthening.
11
Introduction of palliative care and health insurance cov-
Surgical treatment is often directed at correcting the
erage for rare disorders of childhood are recommended
associated deformities rather than restricted to the
to
improve outcome.
exostoses alone. The surgeries may be multiple thus, the
1
psychological effect on the patient should be considered.
Conflict of interest: None
Genetic counselling is an important aspect of the man-
Funding: None
agement of HME as each individual is at 50% risk of
References
1.
Murphey MD, Choi JJ, Krans-
10. Stitzman-Wengrowicz M, Pre-
17. Welsh GA, MacLeod I.
dorf MJ, Flemming DJ,
tell-Mazzini J, Dormans J,
Diaphyseal aclasis affecting
Gannon FH. Imaging of osteo-
Davidson R. Regression of a
the temporomandibular joint.
chondroma: variants and com-
sessile osteochondroma: A case
Dento maxilla fac Radiol
plications with radiologic-
study and review of the litera-
1999; 28: 320- 323.
pathologic correlation. Radio-
ture. University
Pennsylvania
18.
Morton KS. On the question
graphics 2000; 20 : 1407-1434 .
Orthopedic J 2011; 21: 73-76
of
recurrence of osteochon-
2.
Peterson HA. Multiple heredi-
11. Yinusa W, Owoola AM, Esin
droma. J
Bone Joint
Surg
tary
osteochondromata. Clin
IA. Hereditary multiple exosto-
1964; 46: 723-725.
Orthop Relat Res 1989; (239):
sis:
case report. Niger
J Clin-
19. Human L. Diaphyseal aclasis:
222 – 30.
Pract 2010; 13: 218-222.
Review of literature and report
3.
Stieber JR, Pierz KA, Dormans
12. Adelowo O, Adebayo S. He-
of
an unusual case. S
Afr Med
JP. Hereditary multiple exosto-
reditary multiple exostoses in
J 1965; 39: 27-29.
ses:
a current understanding of
two Nigeria siblings. BMJ
20. Vanhoenacker FM, Van Hul
clinical and genetic advances.
Case Rep 2009;
W,
Wuyts W, Willems PJ, De
University Pennsylvania Or-
2009.pii:bcr09.2008.0901 .
Schepper AM. Hereditary
thopaedic J 2001; 14: 39 – 48.
13. Zak BM, Schuksz M, Koyama
multiple exostoses : from ge-
4.
Bovee JV. Multiple osteochon-
E,
Mundy C, Wells DE, Yama-
netics to clinical syndrome
dromas. Orphanet
J Rare
Dis
guchi Y. et
al . Compound het-
and complications. Eur
J Ra-
2008; 3 :3.
erozygous loss of EXT1 and
diol 2001; 40: 208-217.
5.
Richardson RR. Variants of
EXT2 is sufficient for forma-
21. Epstein DA, Levin EJ. Bone
exostosis of the bone in chil-
tion of multiple exostoses in
scintigraphy in hereditary
dren. Semin
Roentgenol 2005;
mouse ribs and long bones.
multiple exostoses. AJR
Am J
40:380-390.
Bone 2011: 48; 979-987.
Roentgenol 1978; 130: 331-
6.
Pannier S, Legeai-Mallet L.
14. Roehl HH, Pacifici M. Shop
333.
Hereditary multiple exostoses
talks: Sugars, bones, and a dis-
22. Crandall BF, Field LL,
and
enchondromatosis. Best
ease
called multiple hereditary
Sparkes RS, Spence MA. He-
Pract Res Clin Rheumatol
exostoses. Dev
Dyn 2010;
239:
reditary multiple exostoses.
2008; 22: 45-54.
1901-1904.
Report of a family. Clin
Or-
7.
Hennekam RC. Hereditary
15. Labram E, Mohan J. Diaphy-
thop Relat Res 1984; (190):
multiple exostoses. J
Med
seal aclasis with spinal cord
217-219.
Genet 1991; 28: 262-266.
compression. Report of two
8.
Schmale GA, Conrad EU 3 ,
rd
cases and review of the litera-
Raskind WH. The natural his-
ture. J
Neurosurg 1996;
84:
tory of hereditary multiple
518-521.
exostoses. J
Bone Joint
Surg
16. Bess
RS, Robbin
MR, Bohlman
Am 1994; 76: 986-992.
HH. Spinal exostoses: analysis
9.
Solomon L. Hereditary multi-
of
twelve cases and review of
ple exostosis. J
Bone Joint
the literature. Spine
1976 2005;
Surg Br 1963; 45:292-304 .
30: 774-780.







