

Copyright 2015 © Nigerian Journal of Paediatrics. All Rights Reserved. . Powered by Pelrox Technologies Ltd
ISSN 03 02 4660 AN OFFICIAL JOURNAL OF THE PAEDIATRIC ASSOCIATION OF NIGERIA


Quick Navigation

Niger J Paediatr 2016; 43 (2):70 – 77
REVIEW
Elusiyan JBE
Hypoglycaemia in children:
Oyenusi EE
Review of the literature
DOI:http://dx.doi.org/10.4314/njp.v43i2.2
Accepted: 16th March 2016
Abstract :
Hypoglycaemia is
a
nosed or undertreated hypoglycae-
common metabolic condition in
mia has been found to increase mor-
Elusiyan JBE
(
)
children. It often presents urgent
tality in children when it is present.
Department of Paediatrics and
and therapeutic challenges and it
This review sought to review the
Child Health, Obafemi Awolowo
University, Ile-Ife. Nigeria.
has been documented to affect
subject of hypoglycaemia in chil-
Email: jelusiyan@yahoo.co.uk
many childhood conditions. Its
dren and calls for testing for it in all
clinical presentation is not classi-
sick and admitted children.
Oyenusi EE
cal and requires a high index of
Department of Paediatrics,
suspicion for an early diagnosis
College of Medicine, University of
and prompt management. Undiag-
Lagos/Lagos University Teaching
Hospital, Lagos, Nigeria.
Introduction
whether ‘asymptomatic’ hypoglycaemia causes neuro-
logical
dysfunction and damage or not.
10
The term hypoglycaemia refers to blood glucose level
The plasma glucose concentration is normally main-
below normal. Most of the time low blood glucose con-
tained within a relatively normal range of 3.9 to
centration is not associated with the development of the
8.3mmol/L (70 to 150mgdl), despite wide variations in
classic clinical manifestations of hypoglycaemia. The
glucose influx and efflux such as those that follow meals
and occur during exercise . There is however general
11
absence of clinical symptoms does not indicate that glu-
cose concentration is normal or has not fallen below
agreement that a value of blood glucose that is less than
optimal level for maintaining brain metabolism. Hypo-
1
2.2mmol/L (40mgdl) represents hypoglycaemia and
most of the work on hypoglycaemia
3,12-14
glycaemia in the paediatric age group is a common clini-
in
the literature
cal finding and is associated with a wide variety of dis-
are based on this cut-off value. Two factors which are
orders . Even in the Tropics, there is a growing aware-
2
frequently overlooked when interpreting the glucose
ness that hypoglycaemia can complicate many child-
concentrations are the analytic method used and whether
hood illnesses. This has necessitated several recent
3
whole blood or serum (plasma) was examined. When
work on the problem of Hypoglycaemia among Nigerian
whole blood is used, the value of blood sugar below
children.
4-6
The
condition often presents urgent diagnos-
2.2mmol/L represents hypoglycaemia as opposed to
tic and therapeutic challenges.
7
2.5mmol/L if plasma (or serum) sample is used. This is
because in individuals with a normal haematocrit, fast-
The major long-term sequelae of severe, prolonged hy-
ing whole blood glucose concentration is approximately
poglycaemia are neurologic damage resulting in mental
8 to
15% less than plasma glucose due to the fact that
retardation, transient cognitive impairment, neurological
the
water content of plasma (93%) is approximately
12%
higher than that of whole blood.
15-17
deficit and recurrent seizure activity. Subtle effects on
8
In
most clini-
personality are also possible but have not been clearly
cal
laboratories plasma or serum is used for most glu-
defined.
9,10
Moderate hypoglycaemia has been shown in
cose determination whereas most bedside methods for
neonates to be associated with a considerable increase in
self-monitoring of glucose use whole blood.
adverse neurodevelopmental effects.
10
Epidemiology
Definition of hypoglycaemia
Hypoglycaemia is said to occur more commonly in pae-
diatric patients than in adults. There are many studies
18
Although there is a general agreement on the need to
maintain blood glucose concentrations above a ‘critical’
on
neonatal hypoglycaemia probably engendered by the
level in young children and neonates, there is no agree-
increased vulnerability of the immature neonatal brain to
damage by hypoglycaemia.
19,20
ment among practising paediatricians and authors as to
the lowest safe concentration of blood glucose.
11
The
difficulty with the definition is understandable in view
Hypoglycaemia has also been reported in children be-
yond the neonatal period
3-6,21
of
the lack of reliable clinical signs when the blood glu-
.
It has been found to also
complicate many emergency paediatric admissions.
3-6,21
cose
concentrations fall in newborn infants and young
children and in view of the continuing controversy over
The
prevalence of hypoglycaemia in emergencies varies

71
from one practice to another.
the brain accounts for almost 100% of total basal glu-
In
Birmingham , a rate of 6.54/100,000 visits was
21
cose turnover making most of the endogenous glucose
found among children seeking care at the emergency
production (EGP) in infants and young children ac-
counted for by brain metabolism , unlike in neonates
1
department while Solomon et al found a rate of 7.1% in
3
Mozambique. More recent studies done in paediatric
where EGP provides approximately one third of glucose
needs. Thus brief hypoglycaemia may cause profound
35
emergency admissions of some West African countries
equally documented the occurrence of hypoglycaemia.
22-
brain dysfunction, while prolonged severe hypoglycae-
24.
mia may eventuate in brain death. Therefore, to main-
11
Prevalence rates of 6.4% in Ile-Ife by Elusiyan et al
22
and 5.6% in Lagos by Oyenusi et al both in Nigeria and
23
tain normal blood glucose concentration and prevent
a
rate of 13% by Ameyaw et al in Kumasi, Ghana re-
24
precipitous falls to levels that impair brain function,
spectively were reported. Other studies such as that done
humans have evolved an elaborate gluco-regulatory sys-
by
Osier et al
25
reported a prevalence of 7.3% among
tem.
11
The prolonged interval between onset of symp-
paediatric admissions in Kenya while a prevalence rate
toms and correct diagnosis reported in most studies indi-
of
18.6% was documented by Wintergerst et al among
26
cates that the possibility of symptomatic spontaneous
patients admitted to a paediatric intensive care unit of a
hypoglycaemia has not received proper consideration
tertiary hospital in California, United States.
early in the course of many clinical situations. There-
fore, whenever repetitive, episodic, bizarre manifesta-
Some authors reported the prevalence of hypoglycaemia
tions occur at any time, whether after a fast, after an
in
studies designed to investigate specific disease enti-
acute illness or shortly after meals, a blood glucose level
ties rather than cohorts ofchildren presenting to the
should be obtained at the time of the symptoms. Only in
emergency room or admitted into the wards with diverse
this way can the diagnosis be established and therapy
problems. For instance, Familusi and Sinnette
27
docu-
instituted early, thus avoiding the sequelae of prolonged
mented aprevalence rate of 13% in children presenting
hypoglycaemia.
36
with febrile convulsions at the emergency ward in
Ibadan, Nigeria. Among children with diarrhoea, the
Elucidation of the physiology of glucoregulation in gen-
prevalent rates of hypoglycaemia reported were 4.5%
eral and of glucose counter regulation in particular has
by
Bennish et al and Bhattacharya et al 40%, respec-
13
28
provided major insights into the pathophysiology of
tively in Asia while in Nigeria, Ntia et al
29
and
Ony-
hypoglycaemia in humans. Nevertheless, there are major
iriuka et al reported prevalence rates of 4% and 4.9%
30
gaps in our understanding of the causes, mechanisms
and management of many hypoglycaemic states. In the
11
respectively.
fasted individual, the maintenance of a normal blood
Another clinical condition in which the prevalence of
glucose level is dependent upon (1) adequate supply of
hypoglycaemia has been widely investigated ismalaria.
endogenous gluconeogenic substrates like amino acids,
Comparable prevalence rates of hypoglycaemia between
glycerol, and lactate (2) functionally intact hepatic gly-
16-17% were documented by English et al
12
in
Kenya,
cogenolytic and gluconeogenic enzyme systems, and (3)
Genton et al in New Guinea and Nwosu et al in La-
31
32
a
normal endocrine system for integrating and modulat-
gos, Nigeria among children with severe malaria. How-
ing these two processes. The adult human being is quite
ever, Onyiriuka et al in Benin, Nigeria and White et al
33
capable of maintaining a normal blood glucose level
in
Gambia
14
reported higher prevalence rates of 18.3%
even when totally deprived of calories for weeks or, in
and 32% respectively in children with severe malaria.
the case of obese subjects, for months. In contrast, the
normal child exhibits a progressive fall in blood glucose
Pathophysiology
to
hypoglycaemic levels when fasted for even short peri-
ods (e.g. 24 to 48 hours).
2,37
The
reasons for the differ-
Glucose plays a central role in mammalian fuel econ-
ence are not clear, but it may be that the young individ-
omy and is a source of energy derivable from glycogen,
ual, when fasting, is unable to supply sufficient glucose
fats and protein. Glucose is an immediate source of
34
to
meet the obligatory demands of the body for glucose.
energy providing 38 moles of ATP/mole of glucose oxi-
Although most tissues have the enzyme systems re-
dized. Blood glucose level reflects a dynamic equilib-
34
quired to synthesize glycogen (glycogen synthase) and
rium between the glucose input from dietary sources
to
hydrolyse glycogen (phosphorylase), only the liver
plus that released from the liver and kidney and the glu-
and kidneys contain glucose-6-phosphatase, the enzyme
cose uptake that occurs primarily in the brain, muscle,
necessary for the release of glucose into the circula-
tion . The liver and kidneys also contain the enzymes
11
adipose tissue and blood elements.
11,34
Hypoglycaemia
thus represents a defect in one or several of the complex
necessary for gluconeogenesis (including the critical
interactions that normally integrate glucose homeostasis
enzymes pyruvate carboxylase, phosphenol pyruvate
carboxykinase, and fructose-1,6- bisphophatase). This
11
during feeding and fasting.
shows the importance of these organs in glucose ho-
The maintenance of the plasma glucose concentration is
meostasis, particularly with gluconeogenesis. In dis-
critical to survival because plasma glucose is the pre-
eased states affecting these organs, hypoglycaemia will
dominant metabolic fuel utilized by the central nervous
be
a major problem unless adequate intake of glucose is
system (CNS) under most conditions. The CNS can
maintained.
neither synthesize glucose nor store more than a few
minutes’ supply of glucose.
11
Glucose metabolism by
There are multiple potential metabolic fates of glucose
72
It
may be stored as glycogen
(deficient endogenus production), or both.
11,38
transported into cells
11
There are
majorly. It may undergo glycolysis to pyruvate, which in
conditions in which glucose utilization is increased
turn can be oxidized to carbon-dioxide and water via the
markedly (e.g. exercise, large tumours, infections) and
tricarboxylic acid cycle, converted to fatty acids (and
in
which renal losses occur at physiological plasma glu-
cose concentration (i.e. renal glycosuria) . However,
11
stored as triglycerides), or utilized for ketone bodies
(acetoacetate, B-hydroxylbutyrrate), or cholesterol syn-
because of the normal capacity of the liver to increase
thesis (Fig.1). Finally, glucose may be released into the
11
glucose production several fold, clinical hypoglycaemia
is
rarely the result of excessive glucose efflux alone.
11
circulation for the immediate metabolic need of the
body. External losses are normally negligible.
11
Rather, it is commonly the result of hepatic glucose pro-
duction that is either decreased absolutely or inappropri-
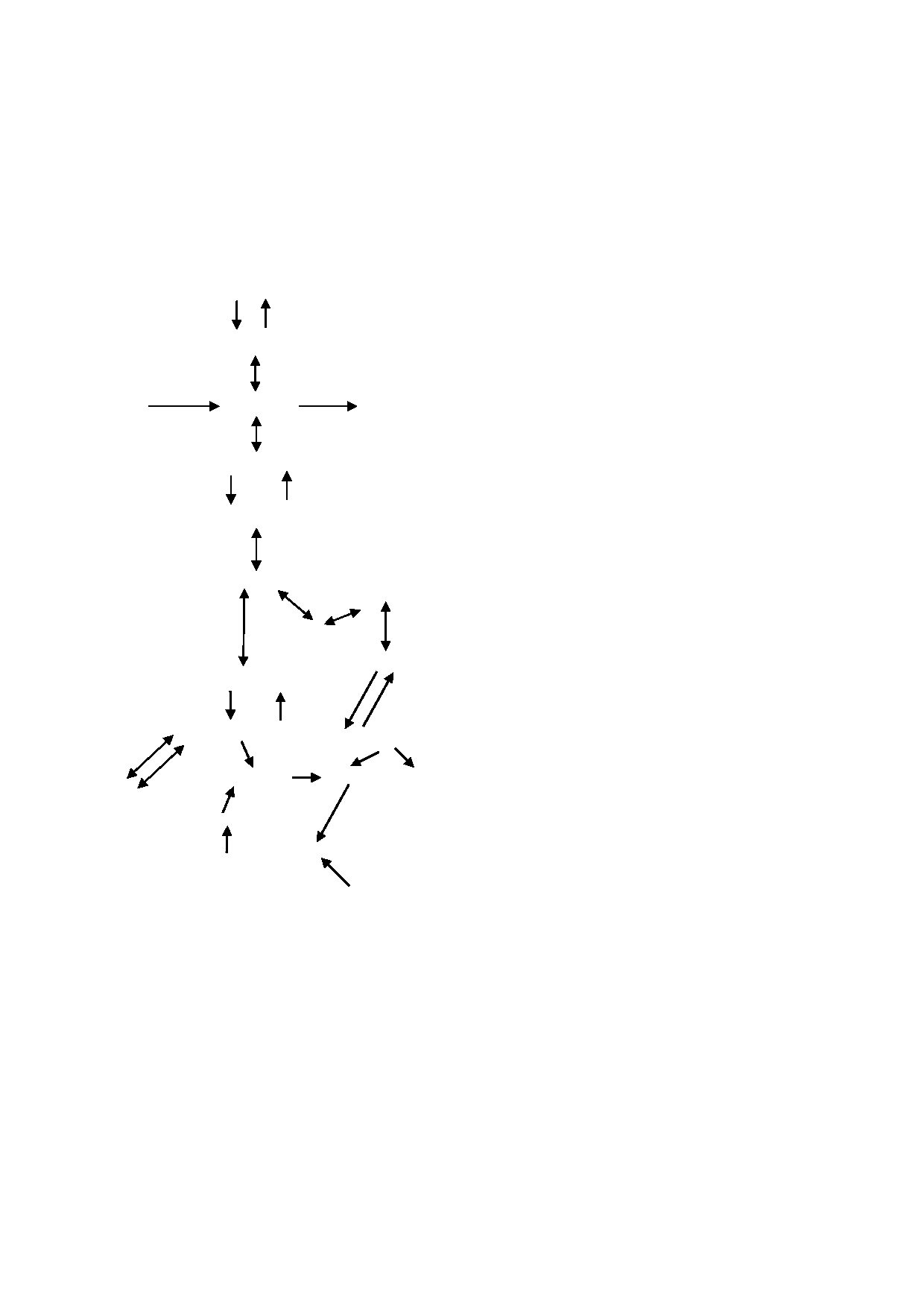
Fig 1: Schematic
representation of
glucose metabolism
11
ately low relative to the rate of glucose utilization .
11
Glycogen
In
African children with malaria and other infections, an
(2)
(9)
impairment in hepatic gluconeogenesis in the presence
of
adequate levels of precursors has been considered the
Glucose-1-p
most likely mechanism
12,14,39
.
(1)
(8)
Other suggested possible mechanisms of hypoglycaemia
in
malaria include accelerated tissue metabolism;
40
Glucose
Glucose-6-P
Glucose
the
metabolic requirements of the parasites and malabsorp-
tion of glucose probably secondary to changes in
Fructose-6-P
splanchnic blood flow owing to a heavy parasite load in
vessels
41,42
.
Sequestration of parasitized red cells in the
(3)
(7)
venules and capillaries of deep tissues may impair local
circulation
43,44
.
This may necessitate a transition to an-
Fructose-1,6-P
aerobic glycolysis releasing lactate and increasing glu-
cose consumption . High serum lactate levels in pa-
45
tients with malaria is thought to indicate lactate produc-
Triose-P
tion by the malaria parasites and anaerobic glycolysis in
TRIGLYCERIDES
tissues where the blood vessels have a heavy parasite
infestation
39,43,46
.
Impaired hepatic gluconeogenesis
GLYCEROL
could also lead to high lactate levels from the Cori cy-
cle . Furthermore, the reduced dietary intake and the
45
FATTY ACIDS
Phosphoenolpyruvate
associated vomiting as well as the increased metabolic
requirement caused by fever in malaria are other sug-
(4)
(6)
gested mechanisms of hypoglycaemia .
14
Pyruvate
AcetylCoA
Mechanisms of hypoglycaemia in infections
(5)
Oxaloacetate
Citrate
KETONES
Hypoglycaemia in other infective process like pneumo-
nia and septicaemia has been attributed to the increased
LACTATE
TCA
cycle
metabolic requirement caused by fever as stated earlier
resulting in increased peripheral glucose utilization.
47
ALANINE
a-Ketoglutarate
Studies have also shown that increased peripheral utili-
zation of glucose appears to be the primary mechanism
Glutamine
for hypoglycaemia in neonates with bacteraemia
48,49
.
Inhibition of gluconeogenesis is considered to be pri-
1.
Hexokinase/Glucokinase
marily responsible for the hypoglycaemia in septicaemia
in
a report by Filkins and Cornell.
50
2.
Glycogen synthase
Endotoxins pro-
3.
Phosphofructokinase
duced by organisms in infectious processes have also
4.
Pyruvate kinase
been known to stimulate increased insulin secretion
causing hypoglycaemia
47,50,51
5.
Pyruvate carboxylase
.
These toxins can also
6.
Phosphoenol pyruvate carboxylkinase
cause hypoglycaemia by contributing directly to deple-
tion of hepatic glycogen stores . Hypotension and de-
47
7.
Fructose-1,6-Bisphosphatase
8.
Glucose-6-phosphatase
creased tissue perfusion in septic shock increase periph-
9.
Phosphorylase
eral utilization of glucose because the shift to anaerobic
from aerobic metabolism requires 18 times more glu-
cose to produce the same amount of energy (ATP) .
52
Mechanisms of hypogyclaemia
Several mechanisms are known to cause hypoglycaemia
Mechanisms of hypoglycaemia in diarrhoeal disease
in
children.
Theoretically hypoglycaemia could result
from excessive glucose efflux (excessive glucose utiliza-
Various factors ranging from hyperinsulinaemia,
tion or external losses), deficient glucose influx
hypoxia, fasting, malnutrition, ketosis and impairment

73
of
gluconeogenesis have been suggested as the mecha-
glucose.
nisms of hypoglycaemia in diarrhoeal diseases
13,50,53
.
2.
Exact cause unknown – Small for gestational age,
Bennish et al noted that plasma levels of counter-
13
fetal distress, any sick newborn Neonatal sepsis,
regulatory hormones (glucagon, epinephrine and norepi-
Neonatal tetanus etc.
nephrine) were appropriately elevated while gluconeo-
B)
Persistent (Neonatal, Infancy and early child hood 0
genic substrates were inappropriately low in the
-2yrs)
children with diarrhoea and hypoglycaemia suggesting
1.
Hyperinsulinism – Islet cell hyperplasia, Nes-
that
the hypoglycaemia observed in such patients is of-
sidioblastosis,
Islet cell adenoma, leucine sensitiv-
ten
due to the failure of gluconeogenesis.
13
ity, Beckwith – Wieldeman syndrome
2.
Glycogen Storage disease
Mechanisms of hypoglycaemia in malnutrition
3.
Defect in gluconeogenesis
4.
Hormone deficiency – Congenital Adrenal Hyper-
During
severe malnutrition, gluconeogenic substrates
plasia, hypothyroidism etc.
such as alanine and lactate are significantly reduced
2,54
.
5.
Miscellaneous – Galactosaemia, Fructose – intoler-
The
capacity to generate glucose by gluconeogenesis is
ance, salycylate intoxication, Reye syndrome, hepa-
markedly diminished and alternate fuels such as ketones
titis
or
lactate are also reduced
2,54
.
The resultant fatty infiltra-
tion of the liver causes glycogen and gluconeogenic
Older Children 1-18 years: The predominant
condi-
substrate depletion. There is also defect in glyco-
tions complicated by hypoglycaemia as seen in the trop-
genolytic pathways and limited lipolysis .
55
ics include severe malaria, septicaemia, pneumonia and
protein-energy malnutrition.
22-25
Other cause
include
Mechanisms of drug-induced hypoglycaemia
side effects of drugs or drug overdosages, use of tradi-
tional concoctions as mentioned earlier amongst others.
Hypoglycaemia can also be caused by medications ad-
Hyperinsulinism, secondary to therapy of diabetes or
ministered to patients in the course of an illness. Drug
islet cell adenoma is also an important cause of hypogly-
therapy for malaria particularly quinine, may cause hy-
caemia.
57-59
poglycaemia by stimulating insulin release
.
The use
of
other cinchona alkaloids like quinidine has also been
Persistent hypoglycaemia
associated with hypoglycaemia . Drug intoxications in
60
children can also cause hypoglycaemia. Excessive doses
There are few examples of persistent hypoglycaemia in
of
salicylates (4 to 6g/day) can distort multiple bio-
children. These include persistent hyperinsulinaemic
chemical reactions to produce metabolic acidosis, hypo-
hypoglycaemia and ketotic hypoglycaemia. It must be
glycaemia or hyperglycaemia
61,62
.
Accelerated utiliza-
pointed out that these classes of hypoglycaemia are
tion of glucose due to augmentation of insulin secretion
rarely reported in the tropics probably due to problems
by
salicylates and possible interference with gluconeo-
with diagnosis.
genesis may both contribute to hypoglycaemia .
62
Accidental ingestion of ethanol is a common cause of
Hyperinsulinaemic hypoglycaemia is a heterozygous
poisoning in children in our environment.
63
In
ethanol
condition in which insulin secretion becomes unregu-
intoxication, the liver metabolizes ethanol as a preferred
lated and its production persists despite low blood glu-
cose levels . It is the most common cause of severe and
15
fuel, and generation of reducing equivalents during the
persistent hypoglycaemia in neonates and children
1,15
oxidation of ethanol alters the NADH/NAD ratio that is
.
essential for certain gluconeogenic steps . As a result,
15
This could be monogenic or syndromic.Congenital hy-
gluconeogenesis is impaired and hypoglycaemia may
perinsulinism (HI) has been described under various
ensue if glycogen stores are depleted . Three to five
15
terms in the past including "idiopathic hypoglycaemia of
percentage of children with alcohol intoxication will
infancy,"
"leucine-sensitive
hypoglycemia,"
or
"nesidioblastosis."
71
have hypoglycaemia . Overdosage of other drugs such
64
It
has now become apparentt that
as
insulin and oral hypoglycaemic agents can also cause
HI
is caused by genetic defects in the pathways that
regulate pancreatic β -cell insulin secretion . Several
71
hypoglycaemia
65,66
.
candidate genes mutations have been identified as re-
Cow’s urine concoction (CUC) is a mixture consisting
sponsible for CHI
including ABCC8, KCNJ11,
GLUD1, GCK, HADH1 .
71
of
cow’s urine, tobacco leaves, garlic leaves, basil
In
a cohort from Tur-
leaves, lemon juice, rock salt and bulbs of onion . It is
67
key,mutations in the ABCC8 gene were found to be the
most common cause of CHI . Management of HI is
72
commonly used in Western Nigeria in the belief that it
controls convulsions or prevents febrile convulsions in
very difficult as current facilities for genetic diagnosis
children but it is known to cause severe hypoglycae-
and appropriate imaging are limited only to very few
mia
27,63,67
.
This could be due to the hypoglycaemic activ-
centres in the world and frequently requires difficult
and garlic contained in the mixture.
70
ity
of onions
68,69
choices, such as near-total pancreatectomy and/or highly
intensive care with continuous tube feedings
71,73
Some
Common aetiology of hypoglycaemia in Neonates
1
patients may respond to treatment with diazoxide, a
A)
Transient 0-7 days
KATP channel agonist while others may also develop
1.
Hyperinsulinism – Infant of Diabetic mothers,
diabetes in later life following the surgery.
erythroblastosis, discontinuation of intravemous
Ketotic hypoglycaemia is said to be the most common

74
76,77
form of childhood hypoglycaemia . It is also referred to
74
diagnosing hypoglycaemia in studies by the authors
.
as
ketotic hypoglycaemia of infancy and classically
A
brand of glucometer was found to have a sensitivity of
manifest between the ages of 18 months and 5 years and
96.00% (95% CI =81.81%-99.80%) and a specificity of
may remit spontaneously before the age of 10 years.
74
96.46% (95% CI=94.17%-98.02%).
76
The predictive
Typical history is of a child who may miss a meal due to
index of a positive test of 64.9% and the predictive in-
dex for a negative test of a 97.72%. An equally high
76
an
infection usually an upper respiratory tract infection
and then develops hypoglycaemia form of childhood
74
specificity (99.8%) and moderate sensitivity (75%) of
hypoglycaemia . It is also referred to as ketotic hypo-
74
another brand of glucometer were observed with high
glycaemia of infancy and classically manifest between
positive predictive and negative predictive values of
94.7% and 98.7% respectively . However it remains
77
the ages of 18 months and 5 years and may remit spon-
taneously before the age of 10 years. Typical history is
74
imperative that at least, a sample should be sent to the
of
a child who may miss a meal due to Convulsion may
laboratory for confirmation. Furthermore, in newborns,
occur at the time of hypoglycaemia and a presumptive
hypoglycaemia should be tested for in all infant of dia-
diagnosis is made by documenting a low blood sugar in
betic mothers irrespective of weight at birth and gesta-
association with ketonuria, ketonaemia and typical
tional age and in all babies born with a birth weight of
4kg and above . Children on nil per
oris too should also
78
symptoms of hypoglycaemia. Ketotic hypoglycaemia is
prevented by limiting the duration of fasting and main-
have regular blood glucose monitoring. Once hypogly-
taining a high glucose intake during illnesses.
74
caemia is diagnosed, blood glucose should be deter-
mined frequently 30 minutes after initial correction and
Clinical features of hypoglycaemia
then hourly, 2 hourly and 4 hourly after obtaining two
normal readings form of childhood hypoglycaemia . It
78
74
The clinical manifestations of hypoglycaemia are non-
is
also referred to as ketotic hypoglycaemia of infancy
specific . In addition, they vary among individuals and
11
and classically manifest between the ages of 18 months
may vary from time to time in the same individuals
11
and 5 years and may remit spontaneously before the age
of
10 years . Typical history is of a child who may miss
74
form of childhood hypoglycaemia . It is also referred to
74
as
ketotic hypoglycaemia of infancy and classically
a
meal due to
manifest between the ages of 18 months and 5 years and
Another benefit of bedside determination of blood glu-
may remit spontaneously before the age of 10 years.
74
cose is to prevent hyperglycaemia which may be caused
Typical history is of a child who may miss a meal due to
by
unnecessary glucose administration to children that
Clinical manifestations of hypoglycaemia fall into two
are normoglycaemic or may even be hyperglycae-
mic
24,25,79,80
categories. The first category includes features associ-
1
.
ated with the activation of the autonomic system and
epinephrine release usually seen with a rapid decline in
Treatment of hypoglycaemia
blood glucose.
1,15
,
These features are sweating, trem-
bling, anxiety, nervousness, weakness, hunger, nausea
The primary objective of treatment is to restore the
blood glucose concentration to the normal range. The
75
and vomiting.
1,15
The
second category includes features
due
to decreased cerebral glucose utilization usually
hypoglycaemic child should receive an immediate bolus
associated with slow decline in blood glucose level or
of
0.25g/kg of dextrose as a concentrated solution (10-
prolonged hypoglycaemia.
15,16
These features are head-
25%) over a minute
1,15,22,23,75,81
.
This should be followed
aches, visual disturbances, lethargy, lassitude, restless-
by
a continuous dextrose infusion at 8-10mg/kg/min in
ness, irritability, difficulty in thinking, inability to con-
order to avoid rebound hypoglycaemia which may occur
within 30 minutes of the bolus injection
1,15,22,75
centrate and mental confusion. Others include somno-
.
Glucose
lence, stupor, prolonged sleep, loss of consciousness,
level should be determined at 15 minutes after the bolus
coma, hypothermia, twitching, convulsion and bizarre
has been given and while the maintenance glucose infu-
neurological signs (motor and sensory), loss of intellec-
sion is running. If hypoglycaemia recurs at this time, a
tual ability, personality changes and outbursts of temper.
bolus of 0.5g/kg of glucose may be given and the
There could also be psychological disintegration with
glucose infusion increased by 25-50% until normogly-
caemia is achieved
15,75
manic behaviour, depression, psychosis, permanent
.
High volume rates carry the risk
mental or neurological damage
1,15
.
of
fluid overload manifest in pulmonary oedema and/or
Therefore it is important to consider the possibility of
heart failure. This can be minimized by the use of a cen-
tral venous catheter and concentrated solutions . Enteric
75
hypoglycaemia in any situation in which the signs or
symptoms are compatible with an inadequate supply of
feeding is encouraged if there are no contraindications.
glucose to the brain .
75
The glucose infusion and blood glucose determination
are discontinued after two consecutive normal blood
Diagnostic work up
glucose levels measured 30 minutes apart and patient is
eating well
22,23
.
Infant of diabetes mothers should be fed
within 30 minutes of birth by the most possible route .
78
Any
child that is sick enough to be admitted to the hos-
pital should be screened for presence of hypoglycaemia.
This
is very important because most times, hypoglycae-
Complications of hypoglycaemia
mia
is asymptomatic and when symptoms are present,
they
are non-specific. Bedside meters have been vali-
A
strong association between hypoglycaemia and in-
dated and found to be highly sensitive and specific for
creased mortality and morbidity has been documented

75
86
by
several authors
3,22-26,82
.
Hypoglycaemia appears to be
thors further noted that the hypoglycaemia of hyperin-
a
function of the severity of illness in childhood and
sulinism is particularly dangerous because it is associ-
more severely ill children will be more likely to die than
ated with total absence of all brain fuels (low plasma
less severely ill ones.
22,23
Hypoglycaemia is also a major
lactate, ketones and glucose) and thus more easily pre-
disposes the individual to brain damage . The risk of
86
indicator of a poor prognosis in different disease entities
like cerebral malaria and gastrointestinal infections
13,29-
brain damage from hypoglycaemia is highest when the
33,39,83,84
.
Hypoglycaemia has been shown to be inde-
hypoglycaemia is prolonged or recurrent and the effects
have been shown to be more in the younger child .
75
pendently associated with speech and language impair-
ments and impairment of non-verbal functioning.
83
Nwosu et al reported that neurological sequelae were
32
about twice as common in children with cerebral malaria
and concomitant hypoglycaemia. The most frequently
Conclusion
occurring sequelae were cortical blindness, monoparesis,
aphasia, hemiparesis, generalized hypotonia, decerebrate
Hypoglycaemia is a common complication of many
syndrome and cerebellar ataxia
33,39
.
childhood diseases with varied pathophysiological
In a
retrospective multicentre study, Lucas et al found
10
mechanisms. It is amenable to treatment but can cause
that moderate hypoglycaemia (<2.6mmol/L) may have
permanent neurological sequelae if prolonged or not
serious developmental consequences if present for five
treated promptly. Children who present in emergency
or
more days during the first two months of life. This
are at special risk of hypoglycaemia. A high index of
provides compelling evidence that even asymptomatic
suspicion should be maintained when evaluating very
86
hypoglycaemia could be harmful . Menniet al
85
re-
sick children for early detection and subsequent prompt
ported that hyperinsulinaemic hypoglycaemia was asso-
and aggressive management.
ciated with psychomotor retardation, learning disability,
seizures and diverse neurological sequelae. The au-
Reference
1.
Sperling MA. Hypoglycaemia. In:
7.
Verrotti A, Fusilli P, Pallotta R,
14.
White NJ, Marsh K, Turner RC, et
Behrman RE, Kliegman RM, Ar-
Morgese G, Charelli F. Hypogly-
al.
Hypoglycaemia in African
ron
AM (Eds). Nelson Textbook of
caema in childhood: a clinical
Children with severe malaria.
Lan-
Peadiatrics, 15 edition. Philadel-
th
approach .
J Pediatr,
Endocrinol-
cet 1987; 1: 708 – 711.
phia. W.B. Saunders, 1996, p 420
Metab 1998; (Suppl 1): 147-52.
15.
Thornton TS, Finegold DN,
–
430.
8.
Jarjour IT, Ryan CM, Becker DJ.
Stanley CA, Sperling MA. Hypo-
2.
Pagliara AS, Kaul IE, Haymond M
Regional cerebral blood flow dur-
glycaemia in the infant and child.
and
Kipnis DM. Hypoglycaemia in
ing
hypoglycaemia in children
In:
Sperling MA (editor) Paediatric
Endocrinology. 2 edn. Philadel-
nd
infancy and childhood. J
Pediatr
with IDDM. Diabetologia
1995;
1973; 82: 365-379.
38: 1090-1095.
phia: Saunders; 2002.pp.135-59.
3.
Solomon T, Felix TM, Samuel M
9.
Bondi FS.. The incidence and out-
16.
Sacks DB. Carbohydrates. In:
et
al. Hypoglycaemia in Paediatric
come of neurological abnormali-
Burtis CA, Ashwood ER(editors).
admissions in Mozanbique. Lancet
ties in childhood cerebral malaria:
TietzFundamentals of Clinical
Chemistry. 5 edition. London:
th
1994; 343: 149-50.
a
long term follow-up of 62 survi-
4.
Elusiyan JBE. Hypoglycaemia in
vors. Trans
R Soc
Trop Med
Hyg
WB
Saunders; 2001.pp.776-85.
Emergency Paediatric admissions.
1992; 86: 17-19R
17.
Ajala MO, Oladipo OO, Fasan-
Dissertation submitted for the
10.
Lucas A, Morley R, Cole TJ. Ad-
made O, Adewole TA. Laboratory
Fellowship of the West African
verse neurodevelopmental out-
assessment of three glucometers.
College of Physician (FWACP).
come of moderate neonatal hypo-
Afr J Med Sci 2003; 32:279-82.
Oct. 2004.
glycaemia. B
M J
1988; 297:
1304
18.
Ltief AN, Schwack WF. Hypo-
5.
Jaja T. Hypoglycaemia in emer-
-1308.
glyaecamia in infants and children.
gency admission at University of
11.
Cryer PE. Glucose homeostatis
Endocrinol Metab Clin North Am
Port Harcourt Teaching Hospital.
and
hypoglycaemia. In: Wilson
1999; 28: 619-46.
Dissertation submitted for the
JD,
Foster DW (eds). Willams
19.
Omene JA. The Incidence of Neo-
Textbook of Endocrinology, 8
th
fellowship of the National Post
natal hypoglycaemia in Benin.
graduate Medical College of Nige-
edition. Philadelphia,
WB Saun-
Niger J Paed 1977; 4: 19-23
ria
(FMCPaed) 2008.
ders, 1992: 1223-1253.
20.
Njokanma OF, Fagbule D. Inci-
6.
Oyenusi EE. Hypoglycaemia in
12.
English M, Wale S, Binns G,
dence, aetiology and manifestaions
children aged one month to 10
Mwangi I, Sauerwein H, Marsh K.
of
neonatal hypoglycaemia. Niger
years admitted to the Children’s
Hypoglycaemia on and after ad-
J Paed 1994; 21: 26-31.
Emergency Centre of the Lagos
mission in Kenyan children with
21.
Pershad J, Monroe k, Atchison J.
University Teaching Hospital.
severe malaria. Q
J Med
1988; 91:
Childhood Hypoglycaemia in an
Dissertation submitted for the
191-197.
urban emergency department:
fellowship of the National Post
13. Bennish
ML, Azad
AK, Rahman
Epidemiology and a diagnostic
graduate Medical College of Nige-
O,
Phillips RE. Hypoglycaemia
approach to the problem.
Paediatr
ria
(FMCPaed) Nov 2011.
during diarrhea in childhood,
Emerg care 1998; 14: 268-71.
Prevalence, Pathophysiology and
22.
Elusiyan JBE, Adejuyigbe EA,
Outcome. N
Engl J
Med 1990;
Adeodu OO. Hypoglycaemia in
a
322: 1357 – 1363.
Nigerian Paediatric Emergency Ward.
J Trop Pediatr; 2006; 52: 96-102.

76
23.
Oyenusi EE, Oduwole AO,
33.
Onyiriuka AN, Peters OO,
45.
White NJ, Warrell DA, Looareesu-
Oladipo OO, Njokanma OF, Ese-
Awaebe PO. Hypoglycaemia at
wan
S, Chanthavanich P, Phillips
zobor CI. Hypoglycaemia in chil-
point of hospital admission of
RE,
Pongpaew P. Pathophysiologi-
dren aged 1 month to 10 years
children below five years of age
cal
and prognostic significance of
admitted to the children emer-
with falciparum malaria: preva-
cerebrospinal fluid lactate in cere-
gency center of Lagos University
lence and risk factors. Niger J
bral malaria. Lancet
1985; 1:776-
Teaching Hospital, Nigeria.
South
Paed 2013; 40:238-242.
8.
Africa J. Child Health. 2014; 8:
34.
Ganong WF. Review of Medical
46.
Kawo NG, Mseng AE, Swai
Physiology 17 edition. Connecti-
th
107-11.
ABM, Chuwa LM, Alberti
24.
Ameyaw E, Amponsah-Achiano
cut: Appleton & Lange;
KGMM, Mclarty DG. Specificity
K,
Yamoah P, Chanoine JP. Ab-
1995.pp.255-89.
of
hypoglycaemia for cerebral
normal blood glucose as a prog-
35.
Tyrala EE, Chen X, Boden G.
malaria in children. Lancet
1990;
nostic factor for adverse clinical
Glucose metabolism in the infant
336:454-7.
outcome in children admitted to
weighing less than 1100grams. J
47.
Miller SI, Wallace RJ Jr, Musher
the
paediatric emergency unit at
Pediatr 1994; 125: 283-7.
DM,
Septimus EJ, Kohl S, Baughn
KomfoAnokye Teaching Hospital,
36.
Bondi FS.. The incidence and out-
RE.
Hypoglycaemia as a manifes-
Kumasi, Ghana. Int
J Paed
Volume
come of neurological abnormali-
tation of sepsis. Am
J Med
1980;
2014, Article ID 149070, 6 pages
ties in childhood cerebral malaria:
68:649-54.
http://
a
long term follow-up of 62 survi-
48.
Yeung CY. Hypoglycaemia in
dx.doi.org/10.1155/2014/149070
vors. Trans
R Soc
Trop Med
Hyg
neonatal sepsis. J
Pediatr 1970;
25.
Osier FHA, Berkley JA, Ross A,
1992; 86: 17-19R.
77:812-7.
Sanderson F, Mohammed S, New-
37.
Senior B, Loridan L. Gluconeo-
49.
Yeung CY, Lee VWY, Yeung
ton
CRJC. Abnormal glucose
genesis and insulin in the Ketotic
MB.
Glucose disappearance rate in
concentrations on admission to a
variety of Childhood hypoglycae-
neonatal infection. J
Pediatr 1973;
rural Kenyan district hospital:
mia
and in control Children. J
82:486-9.
prevalence and outcome. Arch Dis
Pediatr 1969; 74: 529-39.
50.
Filkins JP, Cornell RP. Depression
Child 2003; 88:621-5.
38.
Otto BE, Jarosz CP, Szirer G. Ho-
of
hepatic gluconeogenesis and the
26.
Wintergerst KA, Buckingham B,
meostasis disturbances – hypogly-
hypoglycaemia
of endotoxic
Gandrud L, Wong BJ, Kache S,
caemia in newborns and infants.
shock. Am
J Physiol
1974;
Wilson DM. Association of hypo-
Przeglad Lekarski 2001; 58:79 -
227:778-81.
glycemia, hyperglycemia and glu-
81.
51.
Yelich MR, Filkins JP. Mechanism
cose variability with morbidity and
39. Taylor
TE, Molyneux
ME, Wirima
of
hyperinsulinaemia in endotoxi-
deaths in the pediatric intensive
JJ,
Fletcher A, Morris K. Blood
cosis. Am
J Physiol
1980; 239:
care unit. Pediatrics
2006;
glucose levels in Malawian chil-
E156-161.
118:173-9.
dren before and during the admini-
52.
Nelson DL, Cox MM. The mo-
27.
Familusi JB, Sinnette CH. Febrile
stration of intravenous quinine for
lecular logic of
life. In: David L,
convulsion in Ibadan children.
Afr
severe falciparum malaria. N Engl
Nelson DL (editors). Lehninger Princi-
ples of Biochemistry.3 edn New York:
rd
J MedSci 1971; 2: 135-149.
J Med 1988; 319: 1040-46.
28.
Bhattacharya SK, Bhattacharya
40.
Warrel DA,Veall N,Chanthavanich
Worth; 2000 pp.3-19.
MK,
Dutta D, Garg S, Mukhopadhyay
P,Karbwang J,White JN, Looaree-
53.
Hirschorn N, Lindenbaum J,
AK,
Deb M Moitra A , Nair GB.
Vibrio
suwan S, Phillips RE, Pongpaew
Greenough WB III, Alam SM.
cholerae0139 in Canada. Arch Dis
P.
Cerebral anaerobic glycolysis
Hypoglycaemia in children with
Child 1994; 71:161-2.
and
reduced cerebral oxygen trans-
acute diarrhoea. Lancet
1966;
29.
Ntia HN, Anah MU, Udo JJ, Ewa
port in human cerebral malaria.
2:128-32.
AU,
Onubi J. Prevalence of hypo-
Lancet 1988; 2: 534-8.
54.
Wharton B. Hypoglycaemia in
glycaemia in under-five children
41.
Walter WK, Myron JT. Malab-
children with kwarshiorkor.
Lancet
presenting with acute diarrhoea in
sorption in plasmodium falciparum
1970; 1:171-3.
University of Calabar Teaching
malaria. Am
J Trop
Med Hyg
55.
Akesode FA, Babalola AA. Hypo-
Hospital, Calabar. Niger
J Paed
1972; 21:1-5.
glycaemic response to exogenous
2012; 39: 63-66.
42. Molyneux ME,
Looareesuwan S,
insulin in children with protein
30.
Onyiriuka AN, Awaebe PO,
Menzies IS, Grainger SL, Phillips
energy malnutrition. Niger
J Paed
Kouyaté M. Hypoglycaemia at
RE,
Wattanagoon Y, Thompson
1987; 14:45-9.
point
of hospital admission of
RP,
Warrell DA. Reduced hepatic
56.
White NJ, Warrel DA, Chantha-
under-five children with acute
blood flow and intestinal malab-
vanich P, Loareesuwan S, Warrel
diarrhoea: prevalence and risk
sorption in severe falciparum ma-
MJ,
Krishna S, Williamson DH,
factors. Niger
J Paed
2013; 40:
laria. Am
J Trop
Med Hyg
1989;
Turner RC. Severe hypoglycaemia
384-8.
40: 470-6.
and
hyperinsulinaemia in falcipa-
31.
Genton B, al-Yaman F; Alpers
43.
Luse SA, Miller LH. Plasmodium
rum
malaria. N
Engl J
Med 1983;
MF,
Mokela D. Indicators of fatal
falciparum malaria: ultrastructure
309:61-3.
outcome in Pediatric cerebral ma-
of
parasitized erythrocytes in car-
57.
Hall A. Dangers of high dose qui-
laria: a study of 134 comatose
diac vessels. Am
J Trop
Med Hyg
nine and over-hydration in severe
Papua New Guinea children.
Inter-
1971; 20:655-60.
malaria. Lancet
1985; 1:1453.
national J. Epidemiology 1997;
44.
Macpherson GG, Warrell MJ,
58. Okitolonda
W, Delacollette
C,
26: 670-6.
White NJ, Looareesuwan S, War-
Malengrea M, Henquin JC. High
32.
Nwosu SU, Lesi FEA, Mafe AG,
rell DA. Human cerebral malaria:
incidence of hypoglycaemia in
Egri-Okwaji MTC. Hypoglycae-
a
quantitative ultra structural
African patients treated with intra-
mia
in children with cerebral ma-
analysis of parasitized erythrocyte
venous quinine for severe malaria.
laria seen at the Lagos University
sequestration. Am
J Pathol
1985;
BM J 1987; 295: 716-8.
Teaching Hospital: predisposing
119:385-401.
factors. Nig
Med J
2004; 45:9-13.

77
59.
Jones RG, Sue-Ling HM, Kear C,
71.
Stanley CA.Perspective on the
80.
Oyenusi EE,Oduwole AO,
Wiles PG, Quirke P. Severe symp-
genetics and diagnosis of congeni-
Aronson AS, Jonsson BG, Alberts-
tomatic hypoglycaemia due to
tal
hyperinsulinism disorders. J
son-Wikland K, Njokanma OF.
quinine therapy. J
R Soc
Med
Clin Endo Metab 2016; 101: 815-
Hyperglycemia in acutely ill non-
1986; 79: 426-8.
26.
diabetic children in the emergency
60.
Phillips RE, Looareesuwan S,
72. Güven
A, Cebeci
AN, Ellard
rooms of two tertiary hospitals in
White NJ, Chanthavanich P, Karb-
S,
Flanagan SE. Clinical, genetic
Lagos, Nigeria. PediatrEmerg Care
-
In Press (Accepted 23 Septem-
rd
wang J, Supanaranond W, Turner
characteristics, management and
RC,
Warrel DA. Hypoglycaemia
long-term follow up of Turkish
ber
2014 and published ahead of
and
antimalarial drugs: quinidine
patients with congenital hyperinsu-
print).doi: 10.1097/
and
release of insulin. BMJ
1986;
linism. J
Clin Res
PediatrEndocri-
PEC.0000000000000440
292:1319-21.
nol. 2015 Dec 18. doi: 0.4274/
81.
World Health Organization. Man-
61.
Asindi AA. Poisoning. In:
jcrpe.2408. [Epub ahead of print
agement of the child with a serious
Azubuike JC, Nkanginieme KEO
73. Ghosh
A, Banerjee
I, Morris
infection or severe malnutrition.
AA
Recognition, assessment and
.
(editors). Paediatrics and Child
Guidelines at the first referral level
Health in a Tropical Region. Ow-
management of hypoglycaemia in
in
developing countries. Geneva
erri: African Educational Services;
childhood. Arch
Dis Child.
2015
2000.pp.56-60.
1999.pp. 485-9.
Dec 30. piiarchdischild-2015-
82.
Jaja T, Nte AR, Ejilemele AA.
62.
Fang V, Foye WO, Robinson SM,
308337. doi: 10.1136/archdischild
Post-neonatal hypoglycaemia and
Summer M, Robinson T, Howard
-2015-308337. [Epub ahead of
paediatric emergency room admis-
JJ.
Hypoglycaemic activity and
print]
sions: a study in the University of
chemical structure of salicylates.
J
74.
Haymond MW, Pagliara AS. Ke-
Port Harcourt Teaching Hospital.
Pharm Sci 1968; 57: 2111-6.
totic hypoglycaemia. Clin
Endo-
The Nigerian Health J. 2011;11:19
63.
Asindi AA. Accidental childhood
crinol Metab 1983; 12: 447-62.
-22.
poisoning in Calabar. Niger
J Paed
75.
Cornblath M, Schwartz
83.
Idro R, Carter JA, Fegan G,
1984; 11:19-22.
R.Disorders of carbohydrate me-
Neville BGR, Newton CRJC. Risk
tabolism in infancy.3 edn. Boston:
rd
64.
Ernst AA, Jones K, Nick TG, San-
factors for persisting neurological
chez J. Ethanol ingestion and re-
Blackwell Scientific Publications;
and
cognitive impairments follow-
lated hypoglycaemia in a paediat-
1991.pp.1-53
ing
cerebral malaria. Arch
Dis
ric
and adolescent emergency de-
76.
Elusiyan JBE, Adeodu OO, Ade-
Child 2006; 91:142-8.
partment population .
AcadEmerg
juyigbe EA. Evaluating the Valid-
84.
World Health Organization. Man-
Med 1996; 3:46-9.
ity
of A Bed-Side Method of De-
agement of severe malaria: a prac-
tical handbook. 2 edn. Geneva:
nd
65.
Mayefsky JH, Sarnak AP, Postel-
tecting Hypoglycaemia in Chil-
lon
DC, Daniel C. Factitious hypo-
dren. Ped
Emerg Care;
2006; 22:
WHO; 2000.pp.43.
glycaemia. Paediatrics
1982;
488-90.
85.
Koh TH, Aynsley-Green A, Tarbit
69:804-5.
77.
Oyenusi EE, Oduwole AO,
M,
Eyre JA. Neural dysfunction
66.
Gerich JE. Oral hypoglycaemia
Oladipo OO, Njokanma OF, Ese-
during hypoglycaemia. Arch
Dis
agents. N
Engl J
Med 1989;
321:
zobor CI. Reliability of bedside
Child 1988; 63:1353-8.
1231-1245.
blood glucose estimating methods
86.
Menni F, de Lonlay P, Sevin C,
67.
Oyebola DDO. Cow’s Urine Con-
in
detecting hypoglycaemia in the
Touati G, Peigne C, Barbier
coction: Its chemical composi-
children’s emergency room. Niger
V,Nihoul-Fékété C, Saudubray J,
tions, pharmacological actions and
J Paed 2015; 42 (1):39-43
Robertet J. Neurological outcomes
mode of lethality. Afr
J Med
78.
Wilker RE. Hypoglycemia and
of
90 neonates and infants with
1983; 12:57-63.
hyperglycaemia. Cloherty JP,
persistent hyperinsulinaemic hypo-
68.
Bramachari HD, Augusti KI. Hy-
Eichenwald EC, Stark AR
glycaemia. Pediatrics
2001;
poglycaemic agent from onions. J
(editors).Manual of Neonatal
107:476-9.
Care.5 edn.Pliladelphia: Lippin-
th
Pharm. Pharmacology 1961;
13:128.
cott Williams & Wilkins; 2004.pp
69.
Jain RC, Vyas CR. Hypoglycae-
569-579.
mic
action of onions on rabbits.
79.
Elusiyan JBE, Owa JA. Hypergly-
BMJ 1974; 2: 730.
caemia in ill Nigerian Children- A
70.
Jain RC, Vyas CR. Garlic in al-
study of 13 cases. Niger
J Paed
loxan-induced diabetic rabbits.
Am
2006; 33:8-1.
J Clin Nutri 1975; 28:684-5.







