

Copyright 2015 © Nigerian Journal of Paediatrics. All Rights Reserved. . Powered by Pelrox Technologies Ltd
ISSN 03 02 4660 AN OFFICIAL JOURNAL OF THE PAEDIATRIC ASSOCIATION OF NIGERIA


Quick Navigation

Niger J Paediatr 2016; 43 (2):64 – 69
REVIEW
Okolo AA
Challenges and opportunities for
Okonkwo IR
Ideh RC
neonatal respiratory support in
Nigeria: a case for regionalisation of
care
DOI:http://dx.doi.org/10.4314/njp.v43i2.1
Accepted: 7th December 2015
Abstract :
Background: Neonatal
Results: In
the 1974-1976
era, the
health appears not to have re-
major cause of neonatal mortality
Okolo AA
(
)
ceived the deserved attention in
at
the University of Benin Teach-
Okonkwo IR, Ideh RC
the context of the Child Survival
ing Hospital (UBTH), Benin City,
Department of Child Health,
University Benin Teaching Hospital
Strategies and this must have con-
Nigeria, was birth asphyxia with
Benin-City, Nigeria.
tributed to the non-attainment of
an
attendant perinatal mortality of
Email: angelneneo@yahoo.com
the MDG-4 in Nigeria. Neonatal
80.9/1000 births. The decline in
mortality contributes 40% or more
the
perinatal
mortality
to
to
the current rate of child deaths
33.4/1000 births between 1976 and
globally, with birth asphyxia, pre-
1980 was linked to the introduc-
maturity and its complications and
tion of delivery room resuscitation
severe infections as the leading
with
a reciprocal decline in the
causes. This emphasises the need
incidence of birth asphyxia. There-
to
re-focus on neonatal health.
after, neonatal mortality rate has
Given the state of the economy in
continued to increase. This
the
low- and middle-income coun-
increase could be attributed to a
tries, Nigeria, like most of the
three-fold rise in the proportion of
other countries lack the resources
very
preterm admissions from
required for efficient neonatal
6.5% in 1985 to 19.3% in 2013.
health care with minimal attention
This population of babies is predis-
on
the strategies needed to ad-
posed to Respiratory Distress Syn-
dress the major causes of newborn
drome and respiratory failure.
death.
Neonatal intensive care did not
Objectives: To
assess the
contem-
include respiratory supports until
porary situation of neonatal care
very recently (2013) when the fa-
in
Benin City, Nigeria and exam-
cilities were provided but at high
ine diverse approaches to be
cost to the patient and the health
adopted to provide high level neo-
system.
natal care services aimed at im-
Conclusion: The
strategies re-
proving neonatal survival rates.
quired to address reduction in neo-
Methods: The
trends of
neonatal
natal mortality rates should neces-
morbidities and mortality over the
sarily include neonatal resuscita-
period between 1974 and 2014
tion and mechanical ventilation, all
were studied by reviewing the
within the context of Neonatal
hospital records covering admis-
Intensive Care. In order to provide
sions and weekly mortality
the full range of neonatal intensive
records. The pattern of categories
care services in a resource- con-
of
babies and the causes of death
strained setting such as Benin City,
were recorded. The information
Nigeria, regionalisation of care in
gathered identified the gaps in the
a
stepwise manner is recom-
management strategies for new-
mended, both for improved medi-
borns over the years. Electronic
cal outcomes and economic reali-
databases such as the Medline and
ties.
Pubmed were searched for rele-
vant literatures published between
Key words: Challenges,
Neonatal
1960 and 2015 which might pro-
ventilatory support, Regionalisa-
vide ideas required to fill the
tion of care
gaps.
65
Introduction
The Benin-City Case study
Several studies have highlighted the high rates of infant
Birth asphyxia has been the leading cause of perinatal
8-10
and young child mortalities in sub-Saharan Africa
1-4
mortality since 1974
.
Between 1976 and 1980, neona-
Indeed this is clearly reflected by the fact that majority
tal mortality trends significantly declined with a recipro-
of
these countries did not meet the MDG 4.
5,6
In
an at-
cal drop in perinatal mortality rate (PMR) and a decline
tempt to meet the MDGs, resources were directed into
in
cause-specific mortality in birth asphyxia. This ob-
improving maternal and child health in the last decade.
served decline in PMR rates could be attributed to the
This action contributed to a significant decline in mater-
introduction of basic perinatal health measures in late
nal and child mortality rates but the decline was less for
1975. In the 1980s and the 1990s, neonatal mortality
newborn deaths which also declined but at a very slow
declined due to a decrease in the loss of bigger babies.
pace as maternal health and child survival programs
Specialized teams were available for care in the delivery
room
8-10
received greater attention . Neonatal mortality contrib-
4-6
.
Early use of assisted ventilation was available
utes 40% or more to the current rate of child deaths
in
the mid-1980s but it was not sustained over time.
globally . This emphasises the need to re-focus on neo-
5,6
However, a few babies weighing less than 1000gm were
natal health.
salvaged. The mortality rate for the crop of babies
weighing less than 1000gm was greater than 90% while
Given the state of the economy in the low- and middle-
the mortality rates for babies less than 1500gm was
income countries, Nigeria, like most of other countries,
greater than 60%. Therefore, these group of babies con-
tributed the bulk of neonatal mortalities .
9
lack the resources (material, manpower and financial)
require for optimal newborn care services. Therefore,
the newborn care physicians in Nigeria need to be inno-
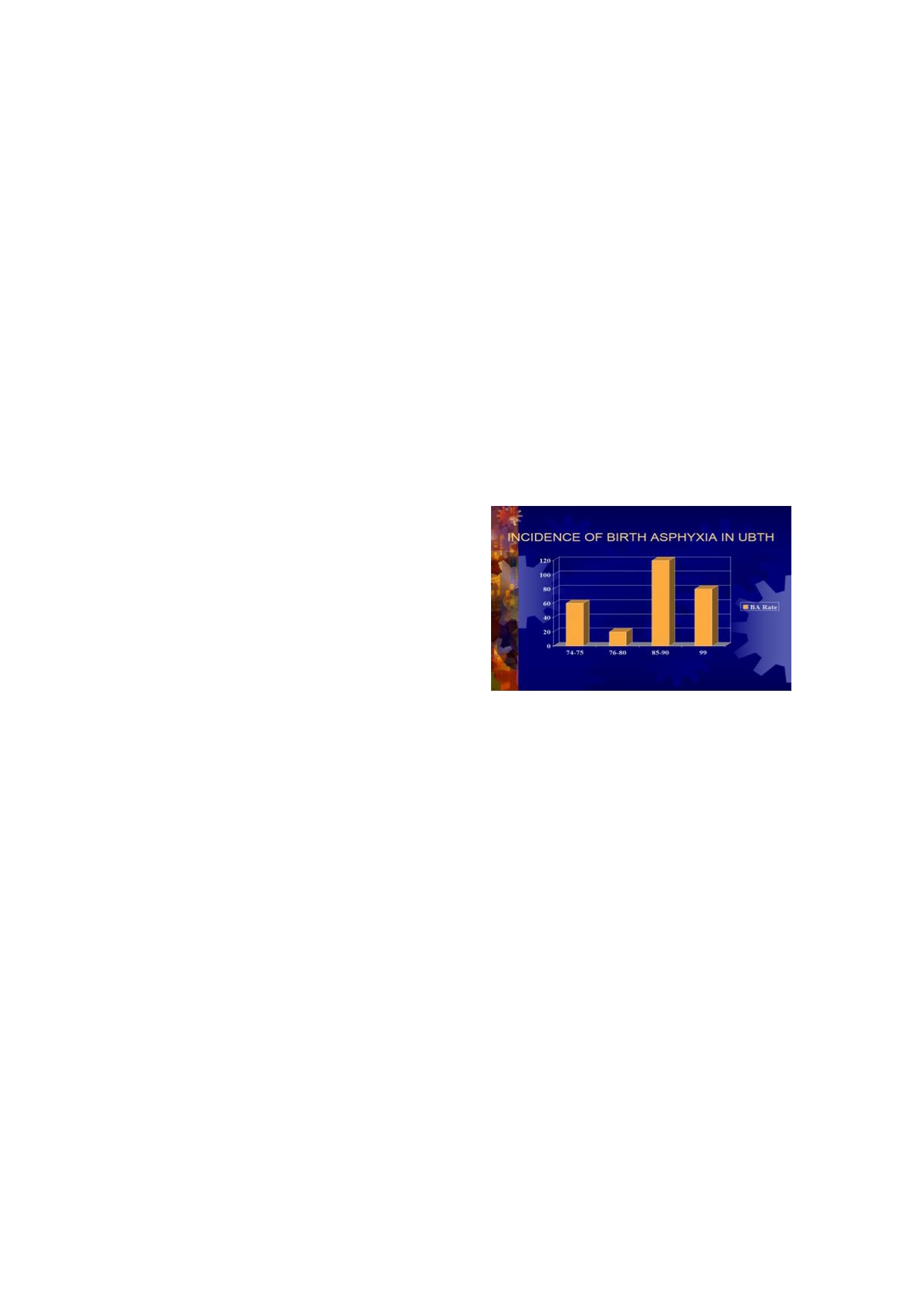
Fig 1: Bar
chart showing
the trends
of the
incidence of
birth
vative, learn to apply the basic principles of child health
asphyxiain Benin City, Nigeria
and adopt a holistic approach in their practices. This
group of practitioners cannot rely too much on the avail-
ability of equipment and other facilities, as it obtains in
the high-income parts of the world, to impact on new-
born care in their setting.
In
the efforts to improve the quality of routine newborn
care, the standard of care provided for sick newborn
infants and improve neonatal survival rates, several new
approaches need to be adopted and adapted to boost the
basic principles of paediatrics and child health. The high
rates of mortality and morbidity among infants and
under-five children accrue from the very high neonatal
By
1990, it was realized that further reductions in neo-
mortality rate (NMR) . The major causes of neonatal
2,5
natal mortality could not be achieved unless attention
morbidities and mortality in Nigeria have not changed
was shifted to the care of the Extremely Low Birth
over time. Birth asphyxia (27%), prematurity and its
Weight (ELBW) infants using intensive care facilities,
particularly, respiratory support
10,11
complications (25%), severe infections (23%) including
.
This management
diarrhoeal diseases (4%), Tetanus (8%) and Jaundice
strategy was instituted in 2013 and small babies are
(8%) are largely responsible for early neonatal deaths in
now ventilated in the context of neonatal intensive care
Nigeria . Efforts to address some of these underlying
6
unit.
causes of mortality among infants and young children
through the Child Survival Strategies (CSS) gave less
Mechanical Ventilation
attention to neonatal health . Other contributory factors
4
like the poor health-seeking behaviour of women , low
7
This form of newborn care often requires other ad-
hospital delivery rate with a low skilled attendance at
vanced modalities of care in the context of neonatal in-
tensive care, which makes it quite expensive . This
11
birth (ranging from 35% to 40%), were not directly ad-
dressed by the CSS.
6,7
form of care is capital intensive both to the health sys-
tem and to the individual patients. The neonatal inten-
In
the past, in Nigeria, only major teaching hospitals
sive care requires ancillary supportive care and efficient
provided neonatal care services including routine care of
team work. Such care, rudimentary as it may be, should
well newborn infants. Although sick babies were cared
be
provided in the context of a minimum standard of
for in the neonatal ward, sophisticated and highly-
care at a Level-II facility. At this level of neonatal care,
specialized neonatal care facilities were not available. In
not only increasing technology is required but also me-
addition, delivery room resuscitation of the newborn
ticulous nursing services, new professional techniques
and team approach . Ideally, oxygen saturation and
12
was not routinely done. Therefore, birth asphyxia, pre-
maturity, sepsis, respiratory disorders and jaundice were
other multiple parameters should be monitored when
the major killers of newborn babies.
8
humidified oxygen is administered to babies, even when
arterial blood gas (ABG) measurement is impossible.
The neonatal intensive care unit team must have the
skills to intubate babies rapidly and provide

66
endotracheal toileting and other supportive care as re-
The scope of neonatal care services in Nigeria: How do
quired. More importantly, skills for the safe and effec-
we meet our needs?
tive use of infant ventilators without causing lung injury
and oxygen toxicity are essential .
13
In
most centres, the care for babies referred from other
health facilities (out-born) is provided largely by differ-
What is Neonatal Intensive care Unit (NICU) and what
ent nurses in a unit that is entirely different from what is
types of Neonatal Units are available?
provided for in-born babies. These units are manned by
nurses with less experience in the care of the newborn
The NICU is an intensive care unit specialized in the
babies thus, high mortality rates in such units may not
care of ill newborns within the first 28days of life. The
be
surprising.
first official Intensive Care Unit (ICU) for neonates was
The rudiments of efficient neonatal care were not avail-
established by Professor Mildred Stahlman at the Van-
able in major centres until about the mid-1960s. In 1974
derbilt University in 1961 . At the same time in the US,
14
precisely, in UBTH, Benin City, the training of paediat-
the first NICU was established and was so recognised
ric resident doctors in neonatal resuscitation and manda-
while Stahlman was the first to use a ventilator to assist
tory attendance at high risk deliveries was instituted.
a
baby with breathing difficulties .
14
This development made significant impact on the New-
In
addition to trained neonatologists, other cadres of
born Mortality Rate (NMR) in the hospital. Newborn
specialist doctors and nurses also work in the NICU as
care was centralised in the same area of the hospital,
necessary. In the least, this group of health workers must
though in different wards. This development was also
be
able to provide neonatal resuscitation. Following the
extended to include the training of nurses to provide
introduction of intensive care into newborn care in the
specialized neonatal care. Today, paediatric residents
US, neonatal mortality has fallen more than four-fold
perform delivery room resuscitation of high risk neo-
from 18.73 per 1000 live births to 4.04 per 1000 live
nates as the standard of care and this has been shown to
15,16
births in 2012
.
Much of this decline can be attributed
have contributed to the decline in the morbidities associ-
to
the highly specialised care provided for preterm and
ated with birth asphyxia at some point. These efforts
sick newborn babies by the neonatologists and the mul-
need to be improved upon to achieve further reduction in
8-10
tidisciplinary teams in the NICU
17,18
.
the
incidence rates of birth asphyxia
.
NICUs are categorised according to the scope of care
What do we have in the other parts of Nigeria?
available in such units. For example, Level-I facility
provides and supports basic care needs of newborn babi-
A
present day challenge is coping with the increasing
es .
While Level-II facility provides special care needs,
12
number of preterm admissions with the decline in the
number of bigger babies requiring admission
8,23
Levels III and IV are more demanding as more material
.
The
and human resources are required to function . These
12
various reasons advanced for the increase in preterm
levels provide comprehensive on-site access to sub-
admissions include increasing use of assisted conception
specialty consultants, performance and interpretation of
and in-vitro fertilisation with high rates of multiple ges-
advanced imaging tests such as computed tomography,
tation, general increase in birth rates, urbanisation,
magnetic resonance imaging and echocardiography on
increase health care-seeking awareness and better utili-
zation of health services for high risk situations
24-27
urgent basis. Other procedures in NICUs include extra-
.
corporeal membrane oxygenation, haemofiltration and
Majority of these babies, as high as 85 to 90%, present
haemodialysis, or surgical repair of major congenital
with varying degrees of respiratory distress culminating
cardiac malformations which require cardiopulmonary
in
respiratory failure and death in more than 50% of
by-pass .
12
such cases.
In
high-income countries, most NICUs now concentrate
How have we met the needs for respiratory support?
on
the care of critically-ill neonates and the very small
infants . Premature labour, and its prevention, remain a
14
How many of the neonatal units in Nigeria provide basic
major challenge for doctors . Even though medical ad-
19
respiratory support using the least device for bubble
vances have made the survival of low birth weight ba-
continuous positive airway pressure (bCPAP)? There are
bies
more possible, it is better to delay such premature
currently very few of our care units equipped to provide
births . No doubt, the use of NICUs have greatly in-
19
basic respiratory support for the newborn. Indeed, the
creased the survival of very low birth weight and ex-
use of the bubble Continuous Positive Airway Pressure
tremely premature infants . In the era preceding the use
20
(bCPAP) as the least respiratory support device is highly
of
NICUs, infants with birth weight less than
limited. There are currently very few neonatal units in
1400 grams rarely survived. Today, infants weighing
Nigeria which use exogenous surfactant for respiratory
500 grams at 24 weeks are known to have a fair chance
distress syndrome among very immature babies despite
of
survival in the more technologically-advanced coun-
the global acceptance of this therapy.The characteristics
tries. Indeed, the NICU environment provides
of
babies in newborn units keep changing; currently, it is
challenges as well as benefits
21,
22
usual to have a mixed population of large sick babies as
well as ELBW babies whose morbidities are variable .
28

67
The constraints to the provision of Respiratory Support
Level-III facilities are available; such NICU should pro-
A
major constrain in the provision of neonatal respira-
vide mechanical ventilation beyond CPAP by nasal
prongs .
12
tory supports is the low level of resources required to
sustain and support such care
17,11
.
Unfavourable Policy environment
Material resources may be insufficient or not available.
The
material resources and equipment required, aside
Policy and management issues are a challenge as rele-
the
ventilators and CPAP machines, include infant incu-
vant
policies are almost non-existence. Neonatal care is
bators, infusion pumps syringe drivers, multi- parameter
capital intensive. Both the overhead cost and mainte-
monitors and ABG monitors. These equipment are very
nance cost are quite high and the returns to service are
expensive . Ventilators, depending on the make, cost on
17
not commensurate with the level of investment made.
the average between five and nine million Naira while
The cost of care is high both to the system and to the
the CPAP machine costs between two and four million
individual patient’s family who often have to pay out -of-
Naira
. Where the ventilators are available, use may be
29
pocket.
hindered by incomplete accessories and lack of concrete
Financial Resources are lacking
11
arrangements for after-sales supports and maintenance.
The equipment may be unsuitable for the environmental
peculiarities in Nigeria, hence they may be damaged by
Financial resources are lacking but resources can be
power outages. On the other hand, the model of equip-
committed, in all its ramifications, to provide the need-
ment may be obsolete and thus, may not be serviceable
ful for ventilator support and care in the context of the
when the need arises.
NICU in Nigeria.
Resources are needed for the development of infrastruc-
Infrastructural arrangements are inadequate
ture, procurement and maintenance of equipment, capac-
ity building and the strengthening of human resources
Most newborn units are not purpose-built and may not
management. Policy and management challenges should
be
in close proximity to the delivery suites in the mater-
be
addressed and social support services should be pro-
nity units. The neonatal units may be space constrained
vided for the users.
and thus, may not have the capacity for mechanical ven-
tilation. Infection control measures may also be difficult
Proposed Solutions include
to
implement. There may also be lack of piped oxygen
or
air or other sources of oxygen supply to the neonatal
The centralisation of care and investment in a concerted
unit. The ambiance may be non-conducive and the unit
effort and approach is desired. This will enable the im-
may have poor air conditioning/ cooling system which is
plementation of a phase approach to the introduction of
unsuitable for the temperature- and humidity-sensitive
change in practices. Regionalisation of such essential
care
12,18
machines and equipment. Some of the equipment are not
which may not be made available at all the cen-
conditioned for harsh tropical climatic conditions and
tres may be a way of reducing costs at the Federal level.
may deteriorate with hot and humid weather conditions.
The States may wish to develop Private-Public Partner-
The incessant power outages affect the electrical compo-
ships to grant the immediate catchment population ac-
nents of machines and indicate the need for back-up
cess to such care. In addition, the state governments may
power sources.
provide Level-II neonatal care.
Un-met human resource needs
The foreseen benefits of the provision of highly special-
ized neonatal care in Nigeria are numerous. In the eco-
Manpower resources are in short supply as there are
nomically advanced countries, investments are made in
insufficient numbers of doctors adequately trained in
the development of care and research. Significant mor-
highly specialised neonatal care to provide the needed
tality from respiratory disorders impaired the attainment
services.
of
the Fourth MDG for most countries of Sub-Saharan
Africa, including Nigeria .
1
Similarly, there is the dearth of nurses trained in neona-
tal intensive care services. This implies inability to meet
If
neonatal mortality must decline considerably, health
the recommended nurse-to-patient ratio for efficient
planners and administrators must invest in the provision
nursing care at the Levels II and III settings .
12
of
ventilator care in the critical care of high-risk new-
born babies . The loss of vulnerable newborns trans-
17
In
addition, there is a dearth of biomedical engineers in
most institutions hence, maintenance services for the
lates to huge economic losses as the nation, by exten-
equipment in the NICU may be difficult to come by.
sion, is deprived of potential manpower for workforce
and economic development .
1,2
When these equipment breakdown, NICU activities
maybe disrupted. This renders support services for ven-
At
the family level, such losses also translate to the im-
tilator care precarious, not prompt, or unavailable. Even
poverishment of the family and a health risk for the
breathing circuits became available in Nigeria, only re-
mothers who would desire another pregnancy to replace
cently, as most centres have been highly dependent on
the lost babies.
the importation of such materials. Indeed, the available
These issues imply increased utilisation of the health
ancillary services are rudimentary. Capacity should be
resources and depletion of economy, which in turn
developed for all level of personnel particularly where
translates to high mortality indicators for the country

68
and shifts the country lower down in the global ranking
there is a cogent need to address the quality of the man-
of
healthy nations. In the Nigerian setting, now is the
1
agement of respiratory morbidities to reduce the mortal-
time to focus on how the need for ventilator support as a
ity arising from them. This can be achieved by providing
crucial part of neonatal care services, could be met and
efficient respiratory support care. The regionalisation of
be
made appropriate for the identified level of care
such highly specialized care at specific tertiary regional
centres may reduce costs whilst secondary level centres
could offer basic respiratory support with the bCPAP. In
the same vein, it is attractive to propose the regionalisa-
Conclusion
tion of full intensive care support for the Nigerian new-
born babies.
The number of preterm babies admitted to neonatal care
units is on the rise coupled with a decline in the number
Conflict of interest: None
of
larger babies requiring hospitalisation. Therefore,
Funding: None
References
1.
State of the World’s Children
10.
Omene JA, Diejomaoh FME.
19.
March of Dimes, Committee on
2008. New York: UNICEF; 2008.
Analysis of 226 asphyxiated new-
Perinatal Health. Toward Improv-
2.
Lawn JE, Cousens S, Zupan J. 4
born infants at the University of
ing
the Outcome of Pregnancy:
million neonatal deaths: when?
Benin Teaching Hospital (1974-
Recommendations for the Re-
Where? Why? Lancet
2005;
1976). Niger
J Paediatr
1978; 5:
gional Development of Maternal
365:891-900.
25-29.
and
Perinatal Health Services.
3.
Oestergaard MZ, Inoue M, Yo-
11.
Kamath BD, MacGuire ER,
White Plains, NY: March of
shida S, Mahanani WR, Gore FM,
McClure EM, Goldenberg RL,
Dimes National Foundation; 1976.
et al .
Neonatal mortality
levels for
Jobe AH. Neonatal mortality from
20.
Bode MM, O’shea TM, Metzguer
193
Countries in 2009 with trends
Respiratory Distress Syndrome:
KR,
Stiles AD. Perinatal regionali-
since 1990: A systematic analysis
Lessons for Low Resource Coun-
zation and neonatal mortality in
of
progress, projections, and pri-
tries. Pediatr
2011; 127:
1139 –
North
Carolina, 1968 – 1994. Am
J
orities. PLoS
Med 2011;
8(8):
1146.
Obstet Gynecol. 2001;184(6):1302
e1001080.
12.
American Academy of Pediatrics,
–
1307
4.
Shiffman J. Issue attention in
Committee on Fetus and Newborn.
21.
Hack M, Wright LL, Shankaran S,
global health: the case of newborn
Levels of neonatal care. Pediatr
et al .
Very low
birth weight
out-
survival. Lancet
2010; 375:
2045 –
2012;130
(3):587 – 597.
comes of the National Institute of
2049.
doi:10.1542/peds.2012-1999.
Child Health and Human Develop-
5.
United Nations Children’s Fund.
13.
Shaffer TH, Alapati D, Greenspan
ment Neonatal Network, Novem-
Committing to Child Survival: A
JS,
Wolfson MR .State of the Art:
ber
1989 to October 1990. Am
J
Promise Renewed. Progress Re-
Neonatal non-invasive respiratory
Obstet Gynecol. 1995;172:457 –
port
2014. United Nations Chil-
support:
Physiological Implica-
464
dren’s Fund (UNICEF) September
tions. Pediatr
Pulmonol 2012;
47
22.
Horwood SP, Boyle MP, Torrance
2014.
(9): 837 – 847.
GW,
Sinclair JC. Mortality and
6.
Federal Ministry of Health. Saving
14.
Stahlman MT. Newborn intensive
morbidity of 500 to 1,499 gram
newborn lives in Nigeria: New-
care: success or failure? J
Pediatr.
birth weight infants live-born to
born health in the context of the
1984;105:162 – 167.
residents of a defined geographic
Integrated Maternal, Newborn and
15.
Mathews T, MacDorman M. Infant
region before and after neonatal
Child Health Strategy. 2nd edition.
mortality statistics from the 2006
intensive care. Pediatr.
Abuja: Federal Ministry of Health,
period linked birth/ infant death
1982;69:613 – 620
Save the Children, JHPIEGO;
data set. Natl
Vital Stat
Rep. 2010;
23.
Martin JA, Hamilton BE, Ventura
2011.
58(17):1 – 31
SJ,
et al. Births: final data for
7.
National Population Commission
16.
Lussky R. A century of neonatal
2009. Natl
Vital Stat
Rep. 2011;60
(NPC) [Nigeria] and ICF Interna-
medicine. Minn
Med. 1999;82
(1):1 – 70.
tional. Nigeria Demographic and
(12):48 – 54.
24. Yoder
BA, Gordon
MC, Barth
WH
Health Survey 2013. Abuja, Nige-
17.
Lee KS, Paneth N, Gartner LM,
Jr.
Late preterm birth: does the
ria, and Rockville, Maryland,
Pearlman MA, Gruss L. Neonatal
changing obstetric paradigm alter
USA: NPC and ICF International.
mortality: an analysis of the recent
the
epidemiology of respiratory
2014.
improvement in the United States.
complications? Obstet
Gynecol.
8.
Omene JA, Okolo AA, Imoe-
Am J Public Health. 1980;70:15 –
2008;111(4):814
– 822.
dehme D, Omu A. Trends in peri-
21
25.
Schieve LA, Ferre C, Peterson HB,
natal mortality rates at the Univer-
18.
Williams RL, Chen PM. Identify-
Macaluso M, Reynolds MA,
sity
of Benin Teaching Hospital,
ing
the sources of the recent de-
Wright VC. Perinatal outcome
Nigeria. East
Afr Med
J
cline in perinatal mortality rates in
among singleton infants conceived
1984;61:461-469.
California. N
Engl J
through assisted reproductive tech-
9.
Omene J.A, Diejomaoh FME.
Med.1982;306: 207 – 214.
nology in the United States.
Obstet
Factors influencing perinatal mor-
Gynecol. 2004; 103(6):1144 –
tality
in a Nigerian community.
1153.
East Afr Med J 1977;54:202-206.

69
26.
Joseph KS, Marcoux S, Ohlsson
28.
MacDorman MF, Kirmeyer S.
29.
Watson AD. Premarket Notifica-
A, et
al , Fetal and Infant Heath
Fetal and perinatal mortality,
tion Decision for Fisher & Paykel
Study Group of the Canadian Peri-
United States, 2005. Natl
Vital Stat
Healthcare Bubble CPAP System.
natal Surveillance System.
Rep. 2009;57(8):1 – 19.
U.S. Food and Drug Administra-
Changes in stillbirth and infant
tion: 510 (k) Number K100011.
mortality associated with increases
2010. Available: http://
in
preterm birth among twins.
tinyurl.com/k100011.
Pediatr 2001;108(5):1055 – 1061.
27.
March of Dimes, PMNCH, Save
the
Children, World Health Or-
ganization (2012) Born Too Soon:
The
Global Action Report on Pre-
term Birth. In: Howson CP,
Kinney MV, Lawn JE, editors.
Geneva: WHO Press. pp 2 – 3.







